Harm Reduction in the Use of Marijuana Part 2 - Atrial Fibrillation
Harm Reduction in the Use of Marijuana Part 2 – Atrial Fibrillation
THE SEARCH BEGINS
For our discussion I will lump everything under “fast heart rate” to keep things simple. That includes everything: palpitations, tachycardia, AF and so on. So, for example, if someone starts smoking pot, and they develop “palpitations” or they feel their heart racing, AF MAY be one of the causes of a fast heart rate, but it will not be the most common cause by any means.
In other words AF appears to be a rare but serious adverse effect from the ingestion of cannabis. How serious? How rare? It’s pretty serious and we hope, rare.
The authors searched the EMBASE AND MEDLINE databases for key words related to our discussion. They found six cases for analysis, only six out of thousands of entries. That’s the good news but the true incidence may be much higher. We simply do not know yet.
Of the six, five required IV pharmacologic intervention to convert AF back to normal sinus rhythm which is pretty disconcerting. None of the cases lasted long, and none of the patients had any serious outcomes other than a syncopal episode (fainting) in two of the patients[ref]Int J Clin Pract. 2008;62(2):308-313[/ref].
The authors continue: Compelling evidence is accumulating that cannabis has significant haemodynamic and electrophysiological effects on the cardiovascular system… mediated mainly by Δ9-tetrahydrocannabinol (THC), although other substances may also be implicated.
These effects include a marked increase in heart rate, lesser increases in supine blood pressure and frequent occurrence of postural hypotension…On the one hand, these effects seem to be dose dependent, but on the other hand, the frequent use over a relatively short period of time results in tolerance.
In the last sentence, tolerance means that the more you smoke the less of an effect you will see as far as tachycardia and postural hypotension goes. Therefore, someone like Willie Nelson probably doesn’t experience ANY tachycardia and hasn’t in 50 years. That’s good news because it tells us that if you don’t experience a tachycardia in your formative years as a budding stoner then you, in all probability, never will. I think this applies to the development of AF as well; once you go chronic, as long as your heart and lungs are in good repair it should not be a problem.
WHO’S AT RISK?
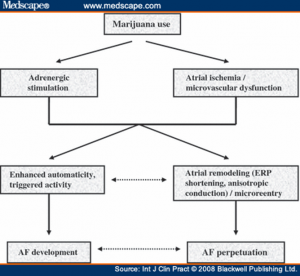
So listen up. The greatest threat is to a novice marijuana smoker (or eater) who experiences the greatest activation of his or her virgin sympathetic nervous system. This can only occur before the vasomotor center (in the brainstem) can “accommodate” to the higher THC levels that frequent users have. Once achieved, it produces a dampening of the brainstem’s sympathetic output, and effectively prevents a tachycardia from developing. This refers to ANY tachycardia including AF (see adrenergic stimulation top left of figure one). This is one case where MORE IS BETTER.
Proposed pathogenesis of marijuana-induced atrial fibrillation. AF, atrial fibrillation; ERP, effective refractory period[ref]IBID[/ref].
From above you can see the author’s proposed model that helps to explain how AF could develop in a marijuana user. AF is a serious disorder which needs prompt medical attention.
To confuse the issue, which is what medicine is all about, many users may in fact be experiencing transient episodes of AF and never know it. But the exact incidence of this disorder is completely unknown at this time. Frequent cannabis users report “palpitations” on numerous occasions but they could be due to sinus tachycardia, AF, PVCs (premature ventricular contractions see section three), or some other as yet to be described dysrhythmia.
The authors also state that the euphoria from marijuana may mask the disconcerting events going on in your chest. Lastly, since pot is still a “dangerous and illicit substance of abuse” many people who might experience a real episode of AF or multiple PVCs may never see a doctor out of fear.
I personally know that this was the case when I was living in Santa Cruz, CA. Here many chronic users came to the Chinese medical clinic for acupuncture knowing they would receive a more sympathetic ear to tell their tales of palpitations.
WHAT TO DO
Now, if you do indeed experience a racing heart rate the first thing to do is get the rate by feeling your pulse on the radial artery on the wrist. Measure it for 60 seconds. That will be your heart rate-simple right?
The normal range of heart rate is about 75 give or take 10 beats on either side. But smoking marijuana clearly increases your heart rate so it might be closer to 100 or more in the apprentice pot smoker. This is called sinus tachycardia and it’s essentially benign. The only problem is that you cannot tell what type it is unless you have an EKG (ECG for you newbies) handy. Interestingly, should your dog get into the brownies he or she will experience bradycardia (a slow heart rate), not tachycardia.
Or you may be having palpitations. The true definition of palpitations is an uncomfortable awareness of your heart (beating). It’s not a true medical term anymore. You may also experience occasional extra beats (premature ventricular contractions, PVCs, ectopy) where you feel your heart flip-flopping; this is what patients often times erroneously call palpitations, but it’s so common that I use the terms interchangeably. Some patients with AF may report having palpitations too.
The impact of marijuana smoking on clinical arrhythmias has not been well studied. Palpitations are commonly experienced after marijuana smoking and are usually ascribed to the sinus tachycardia or more rarely to premature ventricular contractions… Petronis and Anthony, in a large epidemiological study, clearly showed that marijuana smoking is independently associated with increased incidence of palpitations, although the underlying cause of this finding was not clarified[ref]Int J Clin Pract. 2008;62(2):308-313[/ref].
Under rare circumstances you may actually be suffering from angina or a heart attack as seen below:
Interestingly, case reports describing a temporal association between marijuana use and ventricular arrhythmias often implicate myocardial ischaemia as the underlying cause [ref](Int J Cardiol 2005; 104: 230-2. Ann Emerg Med 2003; 42: 365-9)[/ref].
But that would be exceedingly rare, and it most likely would happen to those with known cardiovascular disease.
In conclusion, there are several fast heart rates (sinus tachycardia or AF) and strange sensations (PVCs, palpitations) that marijuana users report usually within the first 90 min of partaking in the cannabis experience. Normally this is of no consequence in young, healthy persons with the exception of AF. Because of the dangers inherent in AF, do not simply assume that your racing heart is of no consequence, that’s called denial.
Should the rate be excessively fast (over 125), sustained for over one hour, or you experience chest pain, lightheadedness, nausea or vomiting it may be signs of something much more serious.
Under those circumstances, the most prudent thing to do is to visit your friendly neighborhood emergency department just to be on the safe side. There they can quickly administer an EKG and “see” what type of cardiac problem you are experiencing. Aside from the fleecing you will receive on your pocketbook (US only of course, not the UK), you will at least be able to sleep that night knowing that you are not one of the few suffering from this dangerous disorder called AF.
Harm Reduction in the Use of Marijuana - Atrial Fibrillation
Harm Reduction in the Use of Marijuana – Atrial Fibrillation
When we compare smoking marijuana to the other “drugs of abuse” we usually give pot a big thumbs up, and paint it in a positive light. And for good reason, marijuana is incredibly safe. Pot’s worst side effects don’t seem worse than tripping over one’s shoelaces, unless you prefer hiking in a Cambodian mine field.
Understandably then, we all tend to gloss over the occasional “chicken littles” of scientific observation when they become known. Such as the much-ballyhooed increase in heart attack risk within one hour of smoking weed. I dispatched that threat quite readily in a previous article. It reminded me of the hit piece, back when people were wearing bell-bottoms, when some malcontent claimed that LSD caused chromosomal damage to users. The article was debunked a week later but there was never a correction issued in the newspaper.
However, substantial evidence is accumulating that smoking marijuana may indeed have a short list of adverse effects that we all need to be aware of, especially young kids experimenting for the first time.
Marijuana’s cardiovascular effects are not associated with serious health problems for most young, healthy users, although occasional myocardial infarction, stroke, and other adverse cardiovascular events are reported. Marijuana smoking by people with cardiovascular disease poses health risks because of the consequences of the resulting increased cardiac work, increased catecholamine levels, carboxyhemoglobin, and postural hypotension[ref]J Clin Pharmacol. 2002 Nov;42(11 Suppl):58S-63S[/ref].
THE DANGERS
The last sentence restates the obvious talking points on marijuana side effects: pot increases blood pressure (only when lying down) while it stimulates the “fight or flight” response-causing tachycardia, a small increase in heart rate. A trivial amount of the oxygen-carrying molecule hemoglobin binds to the by-product of combustion, carbon monoxide (CO), to form carboxyhemoglobin. Carbon monoxide, a poisonous gas formed from combustion of carbon containing materials, is the same substance fashioned from burning charcoal on a grill which is one reason why you cannot light up your Weber Grill in the living room, the other reason is obvious I hope, as any personnel from the LA County-USC burn unit will testify-myself included.
CO is formed from smoking cigarettes or pot too. It can, in larger quantities, impede oxygen transport by competing for oxygen binding sites on hemoglobin. Is it clinically significant? I think not unless you already have underlying cardiovascular or lung disease such as COPD.
Lastly, the postural effects of pot are dizziness when you stand up too quickly. It’s called orthostatic hypotension. Be careful here as people have fainted from this. You can help prevent orthostasis by staying well hydrated, no gin is not a hydration medium, drink water and fluids that behave like water! A little trick I learned as an avid trekker is to put a big pinch of salt in each quart of fluid. This helps keep water in your vessels where it’s needed. Now let’s discuss a more serious problem.
ATRIAL FIBRILLATION (AF)
In particular for kids, err, young adults experimenting with pot, honesty is the best policy so let’s begin with a frank discussion on the cardiovascular system as it pertains in particular to heart arrhythmias (palpitations). In a separate piece I’ll review stroke risk.
A study was completed recently that tried to address the incidence (the number of NEW cases in a given population) of a certain dangerous rhythm disturbance called atrial fibrillation from the use of pot.
Atrial fibrillation (AF) is actually a very common disorder among those with known heart disease, heart failure, or hypertension among other conditions. It is characterized as a fast heart rate, very fast sometimes, with rates well into the high 150s or higher. It is not benign. It can lead to stroke and numerous other serious complications, including cognitive decline.
The question I always ask patients is this: “does your heart sometimes feel like a trip hammer or does it feel like a bird is fluttering in your chest?” Occasionally, severe chest pain may accompany it in those with heart disease.
In the next segment we’ll discuss what a team of researchers discovered regarding AF and its relation to marijuana consumption.
Can Marijuana be used to treat Addiction? - Part 1
Can Marijuana be used to treat Addiction? - Part 1
The next time you are sitting on a park bench listening to the 25th anniversary edition of Tull’s Aqualung, ponder this: why do humans have endogenous ligands in their brains that resemble opium and marijuana biomolecules? How do these systems interact? What are the medical implications? The answers lie in addiction and reward pathways.Read more
Do Endocannabinoids Increase Physical Performance? - Part 2
Do Endocannabinoids Increase Physical Performance? – Part 2
In part one we finished with evidence showing endurance exercise activates the endocannabinoid system in humans. This has been proposed as an explanation for the altered mental status that accompanies intense exercise. Let’s now continue with that line of reasoning.
We know that the endocannabinoid system reduces pain sensations equivalent to that of morphine[ref]2004; Br J Sports Med 2004;38:536-541[/ref]. CB1 receptors have been found in abundance along peripheral nerves that transmit pain sensations as well as in central regions of the brain modulating pain signaling. They also clearly alter emotional states implying that this system may account for some of the effects that exercise produces.
Due to the resolve of scientists over the last decade we now know that there are CB receptors in muscle, skin, endothelial cells (lining blood vessels), and lung tissue suggesting a possible role for this system in mediating certain physiological responses to exercise[ref]IBID[/ref].
EXERCISE
Studies have revealed that exercise suppresses pain, induces sedation, reduces stress, and elevates mood[ref]IBID[/ref]. These are all symptoms of endocannabinoid activation as well. This reinforces a cannabinoid model for helping to explain an exercise induced high.
As a certified gym-rat myself, I unscientifically lumped both the runner’s high and the exercise-induced high together. The latter would be from any form of exercise that is not a repetitive, rhythmic effort such as resistance training, tennis, basketball, heavy bag work, etc. However, the two highs may be quite different in origin.
The runner’s high may have more to do with endocannabinoids. While the run-of-the-mill exercise induced high may have more to do with growth hormone, dopamine, or testosterone release.
It’s clear that both produce a wonderful feeling of contentment and well-being. Yet, the long distance runner can boast an extraordinary type of mental state where one feels omnipotent and ecstatic, even blissful. I have had this experience only during running, and it’s pretty nice I must admit. I can’t approach that delightful state doing Bikram yoga, karate, or resistance training even after hours of high intensity work.
Therefore, it appears as if the cannabinoids might weigh in more for long distance, rhythmic events against gravity (swimming does not produce a runners high). While other contenders such as HGH release, fit the calm sense of well-being from other forms of exercise like peak fitness cycles (running hills for example) or weight training.
Furthermore, the high from weight training for example, kicks in after the event is over not during the actual grunting and straining. The runner’s high clearly occurs during the event and not after. This may be one of the key puzzle pieces needed to ferret out its origins.
Corroborating this idea comes from studies which show that the cannabinoids are activated the most from tissue damage as seen when runners pound their feet for miles.
Bearing on this problem, evidence is accumulating that cannabinoids induce analgesia by acting through CB1 receptors located in skin. This mechanism might suggest that painful stimuli to the skin are particularly potent in activating endocannabinoid antinociception [pain relief][ref]IBID[/ref].
OTHER ACTIVITIES
What about the tissue damage from martial arts or rugby? Clearly we see some serious tissue being thumped when participating in these activities. What do these forms of exercise produce? At this point we do not know what other events produce high levels of endocannabinoids since they have not been studied yet. Only further testing will tell us if the endocannabinoid system is engaged in these different forms of exercise.
However, it’s unlikely that they will demonstrate high endocannabinoid levels since the powerful runner’s high isn’t usually associated with these sports.
As an interesting aside, the only other activity that I can think of that produces a profound sense of bliss is meditation. But doesn’t smoking pot (I’ve read) sometimes do this? In a future article I’ll explore the relationship between the bliss of inner peace through meditation and the endocannabinoid system.
Yet, all types of exercise produce a calm state of well-being. Soon we’ll see that, as we say farewell to the endorphin era and bid adieu to the endocannabinoid age, the cannabinoids will most assuredly play some role in producing it.
Do Endocannabinoids increase Physical Performance? - Part 1
Do Endocannabinoids increase Physical Performance? – Part 1
THE RUNNER’S HIGH
Are you familiar with the term “runner’s high?” It’s the sensation of inner peace milers in particular receive after prolonged running. It’s also sometimes called a second wind. In high school I was involved in track and cross-country sports. I can testify to the incredible feeling I would occasionally, but not always, receive while running. Usually it would happen after many miles of pounding the pavement. Then, unexpectedly, it would hit with considerable force producing a momentous euphoria, and an increase in strength and inner peace. That’s technically what we call the runner’s high. In addition, no other form of exercise seems as reliable in generating this wonderful mental state. Recently, exciting research from the UK has identified the endocannabinoid system as the primary contender for this unusual phenomenon.
Here’s a definition of the runner’s high from Pargman:
Traditionally, the runner’s high has been operationally defined as a “euphoric sensation experienced during running, usually unexpected, in which the runner feels a heightened sense of well being, enhanced appreciation of nature, and transcendence of barriers of time and space”(Pargman et al p.342)[ref]2004; Br J Sports Med 2004;38:536-541[/ref].
THE EXERCISE-INDUCED HIGH
One could also call the sedated, calm, sense of well-being after a typical workout in the gym a type of “runner’s high.” Here it’s simply the nice feeling of peace and relaxation that we get after intense exercise of any type, including running.
Together we can call them exercise-induced highs with the runner’s experience being more powerful, and possibly unique.
RESEARCH
Initially investigators theorized that this phenomenon was due to the release of adrenalin, a “fight or flight” hormone. Then, several decades ago Dr Candice Pert and Dr Solomon Snyder isolated the opiate peptide receptor system. This revelation shocked the world while just missing the Nobel Prize for their efforts. After that everyone claimed that the runner’s high was due to exercise-induced release of “endogenous morphine.” These are opiate-like molecules called endorphins located within regions of the brain involved in cognition and pain relief among others. It seemed the perfect candidate for inducing a “high.” In the decades that followed we also saw human growth hormone (HGH) added to the list. Then came dopamine as it stimulated the reward center in our runner’s brain. Another feel-good contender was serotonin.
However, even though the theory of endorphins dominated as the source for the runner’s high, it has not been able to maintain its elite status. The endogenous opiate system has endured criticism over the years for several reasons. For example, in addition to inducing euphoria, opiates cause respiratory depression, pinpoint pupils and constipation but runners never get those symptoms. In fact, it’s quite the opposite. Running is a sure cure for constipation as any miler will contend. Finally, the scientific community weighed in with some major heavyweights like world authority on opiate peptides Dr Snyder:
Dr Huda Akil and Dr Solomon Snyder—have publicly criticised the hypothesis as being “overly simplistic”, being “poorly supported by scientific evidence”, and a “myth perpetrated by pop culture[ref]IBID[/ref].”
In fact, compelling evidence suggests that an exercise-induced high may be a combination of many endogenous molecules released during and after exercise: namely dopamine, HGH, testosterone, cortisol, serotonin, endorphins and now cannabinoids.
THE ENDOCANNABINOIDS
Recently, with the isolation of the endocannabinoid receptors CB1 and CB2 scientists are able to see this phenomenon in a new light. Maybe the blissful runner’s high is really due to the activation of our endocannabinoids?
Why not? After all, we are seeing an endless stream of research showing how cannabinoids play a role in rewarding pleasurable activities in such diverse systems as alcohol and opiate addiction; pleasure in eating sweet and savory foods; nicotine addiction and so forth. Why not add exercise-induced euphoria to the list?
The proof lies just over the horizon. Recently authorities have revealed with certainty that endocannabinoids play a critical role in exercise:
However, recent data in our laboratory showed that endurance exercise activates the endocannabinoid system, suggesting a new mechanism underlying exercise induced alterations of mental status…we found that exercise of moderate intensity dramatically increased concentrations of anandamide [a THC-like endocannabinoid] in blood plasma[ref]IBID [2004; Br J Sports Med 2004;38:536-541][/ref].
In part two we’ll finish our discussion on the role of exercise and endocannabinoid activation. It appears as if the runner’s high may indeed be an event triggered by our own heady cannabinoids while other forms of exercise induced tranquillity may have their origins in yet other biomolecules hidden within our central nervous systems.
The Effects of CBD on the Human Body, as explained by a Doctor
One of the most celebrated elements found in cannabis is a chemical called CBD which is short for cannabidiol. It is a non-psychoactive compound that is a powerful anti-inflammatory, anti-spasmodic, and anti-seizure medication. Yet, its list of accolades doesn’t end there.
So far, the endocannabinoid system (meaning endogenous cannabinoid) is the largest receptor system known to exist in the human body. It’s a system that helps to maintain homeostasis, to keep things running in tip-top shape. That means that we already have our own versions of pot molecules in our nervous systems.
That alone is extremely interesting. It accompanies a growing list of psychoactive elements found in our brains such as PCP, DMT, opiate, and Valium-like molecules among others. The correlation of human neurotransmitters with plant molecules is perhaps one of the most baffling, yet intriguing, discoveries ever made. Now we can add endocannabinoid molecules acting as neurotransmitters in our brains and peripheral nerves.
Let’s examine just how this interesting little molecule exerts its effects. The endocannabinoid system so far has two known receptors, the CB 1 & 2, with a possible third candidate the GPR55 receptor system. CB 1 is mostly found in the brain while CB 2 is in the peripheral nervous system. CBD has a complicated portfolio of direct and indirect actions both centrally and in peripheral nerves.
We now know that CBD acts as a weak antagonist (it blocks the receptor) on CB 1. Recently it was revealed that CBD has a stronger antagonist effect on CB 2 within the endocannabinoid system in humans.
Classically, CBD antagonizes these receptors but it indirectly stimulates endogenous cannabinoid signaling by suppressing fatty acid amide hydroxylase (FAAH), which is the enzyme that metabolizes anandamide.
Anandamide is an endogenous cannabinoid that activates the CB1 receptor. CBD therefore, indirectly leads to increased CB1 signaling through increasing the quantity of anandamide at the receptor in spite of the fact that CBD weakly antagonizes CB1. The end result may be to stimulate the system. Stimulating CB 1 is where the “high” from pot smoking comes from. Incidentally, CBD in excess quantities, may decrease the high from THC since it is an antagonist of CB1.
But wait there’s more to it. CBD also stimulates the release of 2-AG another endogenous cannabinoid which stimulates both CB1 and CB2 receptors. In the final analysis the effects are a complicated symphony of stimulation and suppression leading to the classic experience of smoking or ingesting marijuana, or to the pain relieving effects of ingesting CBD preparations.
Looking at the figure below we see that CBD also acts as an agonist at the 5HT1a receptor (the serotonin receptor where LSD works), and an agonist at the vanilloid receptor known as TRPV-1.
Lastly, it also stimulates adenosine receptors. One of which acts as a powerful anti-inflammatory known as A2A. Don’t forget that CBD is a potent antioxidant in its own right. The ability of CBD to quench free radicals is more powerful than vitamin C or E. Free radicals have been implicated in dozens of disorders including the aging process itself. If we combine CBD with THC we see even greater antioxidant effects[ref]CBD: How It Works. Martin A. Lee. (PDF O’Shaughnessy’s Autumn 2011)[/ref].
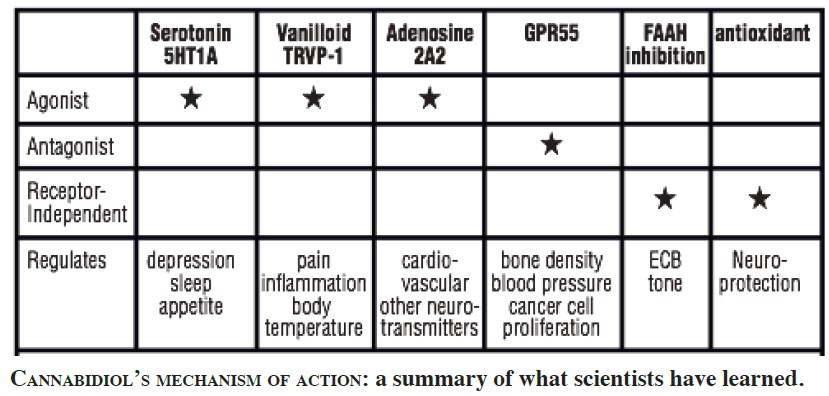
Figure 1 CBD How it works from Martin A Lee (O’Shaughnessy’s • Autumn 2011)
As you can see from the above table there are six systems where we know CBD acts. It stimulates serotonin, vanilloid and adenosine receptors leading to possible applications in treating depression, insomnia and appetite (serotonin); reducing pain and inflammation (vanilloid); and in the treatment of cardiovascular disorders (adenosine) respectively. By antagonizing (blocking) the GPR55 system possible applications are in the treatment of osteoporosis, high blood pressure, and cancer metastasis especially with breast cancer.
Lastly, during myocardial ischemia the heart often times misbehaves and can develop serious rhythm disturbances such as ventricular tachycardia (V-tach). In a rat model CBD was shown to decrease the incidence of V-tach during coronary artery occlusion[ref]British Society for Cardiovascular Research doi:10.1136/heartjnl-2011-301156.17 Y Hepburn, K Walsh, L Wainwright. The Robert Gordon University, School of Pharmacy and Life Sciences, Aberdeen, UK; (web: http://cannabisclinicians.org/cannabidiol-cbd-as-an-anti-arrhythmic-the-role-of-the-cb1-receptors/) 11/24/2014[/ref] but just how it does that remains a mystery.
There is still much needed work to be done before we’ll have it clear as to the role of cannabinoids in treating the numerous expressions of inflammatory diseases. To do that we’ll need to get pot removed from its current schedule I status to at least schedule II so that research dollars can pour into the system.
Finally, let’s take the trillions wasted in drug interdiction and the prison system for non-violent drug offenders toward research into cannabinoids. If we do that you got yourself a “Going Jesse.” It only makes one wonder what bounty might already be available to our moribund masses had President Nixon or Carter legalized marijuana back when they should have.
Regardless of where the chips finally fall there’s much promise in the years to follow.
The Use of Cannabis in the Treatment of Opiate Addiction
The Use of Cannabis in the Treatment of Opiate Addiction
Did you know that we have a powerful and highly effective method for opiate addicts to safely detox from their addiction?
It does not involve the leading methods currently used by mainstream addictionology. Rather, it involves the use of a currently illegal substance: marijuana.
Treating opiate addiction with an illicit drug like cannabis is a controversial practice. Strangely enough, addictive and dangerous medications like methadone and Suboxone, manage to evade scrutiny while non-addictive alternatives such as cannabis (and ibogaine, see below) therapy is still awaiting a green light from our “thought leaders.”
The use of medical marijuana in treating addiction boasts a laundry list of anecdotal reports, successful animal studies, and clinical trials, but social and legal criticism still inhibits serious discussions on the medical use of pot for opiate detoxification. This needs to change because we have a huge addiction problem in the developed world, especially in America the leader in polypharmacy.
WE HAVE A PROBLEM
In the US there are between 600,000 and 1.5 million heroin addicts reported for 2010[ref]http://www.forbes.com/sites/jacobsullum/2014/03/10/how-many-daily-heroin-users-are-there-in-the-u-s-somewhere-between-60000-and-1-million-maybe/) 04/14/2015[/ref]. It is estimated that between 26.4 million and 36 million people abuse opioids worldwide, with an estimated 2.1 million people in the United States suffering from substance use disorders related to prescription opioid pain relievers in 2012[ref]America’s Addiction to Opioids: Heroin and Prescription Drug Abuse, May 14, 2014, presented by Nora D. Volkow, M.D. (Original: Senate Caucus on International Narcotics Control UNODC, World Drug Report 2012. http://www.unodc.org/unodc/en/data-and-analysis/WDR-2012.html)[/ref]. In Europe, 1.3 million people are addicted to heroin, the primary drug for which treatment requests are sought[ref]Front Pharmacol. 2015; 6: 6.[/ref].
The landscape started to change in the early part of the 21st century. By 2002, death certificates listed opioid analgesic poisoning as a cause of death more commonly than heroin or cocaine[ref](http://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2014/americas-addiction-to-opioids-heroin-prescription-drug-abuse#_ftn10) 04/21/2015[/ref].
We have two separate groups needing help: the immense numbers of patients hooked on pharmaceutical opiates, and a much smaller number of heroin addicts. As a way to curb heroin addiction, some people choose to enroll in the federal methadone maintenance program. This treatment alternative is not a cure, you are simply replacing one opiate for another. However, methadone may be far worse than we thought. Deaths from methadone overdose are skyrocketing even with opiate tolerant addicts.
According to CBS News, methadone accounts for only 2 percent of painkiller prescriptions in the United States. However, the drug accounts for more than 30 percent of prescription painkiller overdose deaths, the Centers for Disease Control and Prevention announced[ref](http://www.cbsnews.com/news/methadone-to-blame-for-one-third-of-us-prescription-painkiller-deaths-cdc-says/) 04/19/2015[/ref]. I personally know of three patients who died from accidental methadone overdoses.
MEET DANNY
What you are about to read is an example of what the enlightened medical community has been doing for years. Mainstream medicine has little to no knowledge of the most powerful approach available for those strung out on opiates, cocaine or methamphetamine. They prefer to cling to outdated therapies that offer little more than high relapse rates.
I am presenting a real case study from my files of a patient I had treated for opiate dependence. It’s beyond the scope of this article to get into the details of his treatment but I will relate to you the main points of this approach.
Danny was strung out. At 38 years old he had managed to dispatch nearly a gram of Demerol (a powerful and highly addicting opiate medication), or the equivalent in heroin, per day for his habit just to remain normal. He was now entering his fourth year as an addict.
Danny had ruptured two disks in his back 4 years earlier leading to severe chronic low back pain. At first he was using the prescription pain reliever Vicodin which quickly became his gateway to more powerful drugs. Soon Danny was out of control as he doctor shopped and sought out black market opiates. When I saw him he was desperate “I can’t keep living like this, it’s stealing my life away,” he told me. By then he had already lost his job.
Lucky for him he lived in California where the medical use of cannabis was legal. I used several different drugs to aid in withdrawal including clonidine and Lomotil. But the game changer was the use of marijuana, without which his chances of a successful detoxification would have plummeted.
The entire process of withdrawal technically took about 6 weeks. In ameliorating the core withdrawal effects-the ineffable anguish that accompanies opiate withdrawal-smoking marijuana was a godsend. It seemed to stimulate the very opiate receptors that were screaming for Demerol leading to the reversal of symptoms like dysphoria, anxiety, and pain. The powerful symptoms that usually prevent an addict from trying to detox.
Danny’s story is astonishing, yet typical of cases using pot for opiate withdrawal. Each morning began with a dose of the above pharmaceuticals which were administered throughout the day. Whenever he “started to feel his skin peeling off his body,” as he described it, he would light up a bowl of cannabis and puff away until the symptoms of withdrawal resolved-usually in about ten to twenty minutes. This would leave him in a comfortable, calm, and relaxed state for about 4 hours. This is a condition far removed from the agony and frenzied anxiety seen in withdrawal where seconds feel like hours. Danny continued this process every time symptoms would reappear. Often up to 6 or more times a day. Over several weeks this ritual worked magically until one day he finally detoxed to a point where he was no longer in withdrawal. Truly his addiction was conquered, and it was a far less brutal and much more effective way to recover.
Danny’s case is one example of thousands of successful applications in the treatment of opiate addiction using marijuana. By replacing opiates with cannabis the risk of relapse decreases while the chances for successful detoxification increase dramatically.
This may be one of marijuana’s best uses to date. People need to be aware of such promising therapies. The reasons are simple. We have a nation of narcotic addicts, mostly from the prescription uses of opiates. It is spiraling out of control.
In the second part of this series we’ll explore this time bomb while we review some of the literature which supports the use of pot in treating not just opiate addiction but methamphetamine and cocaine use as well.
The Use of Cannabis as a Potent Anti-Inflammatory - Part 4
The Use of Cannabis as a Potent Anti-Inflammatory – Part 4
CANNABIDIOL (CBD)
In part three we discussed the exciting results of several studies using cannabis ligands for their plaque punching potency in treating inflammation (atherosclerosis) via the CB system. In this final installment we’ll explore the uses of CBD, an amazing phytocannabinoid. Furthermore, CBD may exert some or all of its anti-inflammatory effects outside of these receptors. From Mohanraj Rajesh et al:
Consistently, CBD has been shown to exert anti-inflammatory and antioxidant effects both in vitro (test tube) and in various preclinical models of neurodegeneration and inflammatory disorders, independent from classical CB1 and CB2 receptors [11 citations].
Cannabidiol has been shown to be effective in protecting endothelial function and integrity in human coronary artery endothelial cells (HCAECs). The study demonstrated that CBD reversed the harmful effects of high glucose on HCAECs by inhibiting: Reactive oxygen species production by mitochondria, NF-κB activation, Transendothelial migration of monocytes, Monocyte–endothelial adhesion in HCAECs.[ref]Mohanraj Rajesh et al., Cannabidiol attenuates high glucose-induced endothelial cell inflammatory response and barrier disruption. Am J Physiol Heart Circ Physiol. Jul 2007; 293(1)[/ref]
Cannabidiol (CBD) is not psychoactive due to a low affinity for the CB1 & CB2 receptors[ref]IBID[/ref]. It has been approved for the treatment of inflammation, pain, and spasticity associated with multiple sclerosis in humans since 2005[ref]IBID[/ref].
In what can only be described as astonishing, Mohanraj Rajesh and his team were able to demonstrate that CBD may be the perfect anti-inflammatory for diabetics and cardiac patients. Its healing effects are so broad as to make one question the authenticity of this study. Basically CBD suppressed all of the adverse effects from excess serum blood sugar that they examined such as hyperglycemia induced free radical damage from NF-kB activation, and superoxide formation. Superoxide, a type of free radical, plays a significant role in the pathogenesis of diabetes-associated endothelial dysfunction[ref]IBID[/ref].
We demonstrate that CBD attenuates HG [hyperglycemia]-induced…superoxide generation, NF-κB activation,…and disruption of the endothelial barrier function in [human coronary artery endothelial cells] HCAECs by a mechanism independent from CB1 and CB2 receptors[ref]IBID[/ref].
Considering that over 80% of the American population has fasting blood sugars above the ideal range (83-85 mg/dl), CBD may be a welcome addition to our paucity of anti-inflammatory/diabetic medicines.
In other words this study shows that CBD may behave as an antidote to diabetic hyperglycemic complications, and in those patients with prediabetes or who eat excessive quantities of refined carbohydrate.
In the conclusion of the above study the author’s state: Collectively, our results suggest that the nonpsychoactive cannabinoid CBD have significant therapeutic benefits against diabetic complications and atherosclerosis.
One study indicates that blocking CB2 also decreases inflammation. While scientists elucidate the role of CB2 stimulation leading to a decrease in the inflammatory response in plaque formation, others are finding that blocking the CB2 receptor with CBD leads to a decrease in the immune response. The authors suggest that these findings may lead the way toward development of a new class of anti-inflammatory drugs[ref]British Journal of Pharmacology (2008) 153, 199–215; 2008 Nature Publishing Group[/ref].
Turning now to CBD, an important recent finding is that this cannabinoid displays unexpectedly high potency as a CB2 receptor antagonist and that this antagonism….can ameliorate inflammation…raises the possibility that CBD is a lead compound from which a selective and more potent CB2 receptor inverse agonist [a type of antagonist] might be developed as a new class of anti-inflammatory agent[ref]Br J Pharmacol. Jan 2008; 153(2): 199–215[/ref].
It is outside the scope of this article to list all of the astonishing effects of CBD in the human body. But I’ll give you a hint: they all seem to be helpful! I will run an article soon which demonstrates the vast syllabus of physiological effects from CBD administration. Now let’s see what the critics love to quote when bashing marijuana.
DARK HORSE: CANNABINOIDS AND HEART ATTACK
Just when you thought it was safe to light your spliff, dribble a single malt, and watch The World’s End for the fifth time, there remains a dark horse in the use of pot and heart disease. At least one study is getting plenty of press. They found that pot smoking increases the risk for heart attack within the first hour of smoking[ref]Mittleman MA1, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001 Jun 12;103(23):2805-9.[/ref]. Now, before your pants catch fire, I think we can discount the publication. This was a retrospective study involving a questionnaire on frequency of marijuana use (with pot heads no less) which makes it notoriously unreliable.
In summary, I have presented compelling animal, tissue culture, and human studies that strongly support a role for cannabinoids in moderating inflammation in general, and specifically in the treatment of cardiovascular disease which includes stroke, heart attack, and pulmonary embolus, our top killers. Drug companies do not currently have ways to treat chronic inflammation which is one of the reasons why industrialized nations have become so sick. Changing one’s lifestyle, preventing inflammation, is currently our only option. But, that’s a tough sell. We may soon see the day when your family doctor instead tells poor Mabel to smoke hash or try some new darling cannabinoid medication.
That’s why a new cannabinoid anti-inflammatory class of drugs would be embraced. Because of their unique, novel, and powerful, systemic anti-inflammatory actions, these drugs could be applied as antidotes to destructive habits, and environmental toxins that are recognized risk factors. These factors are not just for atherosclerosis but also for cancer, and neurodegenerative diseases like Alzheimer’s disease and Parkinson’s disease which are reaching pandemic proportions.
Furthermore, these novel compounds, and many more just waiting for a fresh, bushy-tailed, research fellow to expose, appear to work far upstream of the inflammatory cascade right into the very heart (pun intended) of cellular inflammation: the suppression of NF-kB. By suppressing NF-kB, a real cure for atherosclerosis could be realized, and with it cures for cancers, neurodegeneration, and a hundred more diseases of affluence. Is this really possible? Indeed. Let me leave you with one of the most profound statements I have come across in my 25 years in clinical medicine and teaching:
…cannabis is a source not only of D9-THC, CBD and D9-THCV but also of at least 67 other phytocannabinoids and as such can be regarded as a natural library of unique compounds. The therapeutic potential of many of these ligands still remains largely unexplored prompting a need for further preclinical and clinical research directed at establishing whether phytocannabinoids are indeed ‘a neglected pharmacological treasure trove’ (Mechoulam, 2005)[ref]Journal of British Pharmacology (2008) 153, 199–215; 2008 Nature Publishing Group[/ref].
Read the first 3 parts of Dr. Rasmussen’s incredible articles here:
The Use of Cannabis as a Potent Anti-Inflammatory Medication - Part 3
The Use of Cannabis as a Potent Anti-Inflammatory Medication – Part 3
In part 3 of this article. we’ll continue on our informative journey through the labyrinthine rabbit hole of current medical marijuana research as it pertains to slaking inflammation. Once again I’ll refer to atherosclerosis as our “model” of inflammation. This is perhaps marijuana’s greatest application. If it can help with cardiovascular disease it will also affect many apparently unrelated disorders.
When I speak of inflammation, think “immune system.” One of the most vital components of immunity is an unassuming cell called the monocyte. When signalled to do so, this cell becomes a voracious eater of many things harmful to the organism. This “big eater” or macrophage (in science speak) plays a fundamental role, in this case in the blood vessel where plaque forms. These cells cause the inflammatory response that is decimating first-world inhabitants en masse.
BLOCKING CB1, AND STIMULATING CB2 IS GOOD FOR YOU
The same team I referred to in part 2 found that antagonizing (blocking) CB1 leads to decreased expression of several key inflammatory markers intimately involved in the generation of plaque. Sugamura et al, demonstrated using cultured human macrophages that antagonizing CB1 led to a decrease in the expression of an enzyme known to induce heart attack and sudden death, the MMP-9 enzyme[ref]Sugamura K, Sugiyama S, Nozaki T, et al. Activated endocannabinoid system in coronary artery disease and antiinflammatory effects of cannabinoid 1 receptor blockade on macrophages. Circulation. 2009;119:28–36[/ref]. There are about 15 risk factors, or what I call Irritating Agents (IA), for atherosclerosis. They include bad habits (nicotine & sloth) or foods (sugar, omega 6 oils) that lead to increased expression of MMP-9 from macrophages. These immune cells, located within the core of an atheroma (plaque), produce this enzyme via CB1 receptor activation which can erode the thin cap covering a young atheroma causing it to burst.
You might say who cares? Well, I care and here’s why: the rupture of a Toxic Atheroma, which happens thousands of times a day all across the developed world, can directly lead to sudden death, stroke, or heart attack.
While agonizing (stimulating) CB2 receptors using very low doses of THC (1 mg/kg/day), Steffens et al[ref]Steffens S, Veillard NR, Arnaud C, et al. Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice. Nature. 2005;434:782–786[/ref] showed an inhibition of progression of atherosclerotic lesions by decreasing monocyte activity via activation of CB2 receptors on these cells. Monocyte infiltration into the blood vessel is a hallmark for atherosclerosis. When they transform into macrophages they gobble up oxidized LDL cholesterol (the ‘bad’ cholesterol) in an effort to contain the damage.
Here’s another new term. The endothelium, is the single cell layer lining all blood vessels. The absence of endothelial dysfunction, is necessary to prevent atherosclerosis. Imagine the endothelium as the Appian Way of blood vessels: each endothelial cell is similar to one of the precision placed paving stones. IA’s injure these “stones” and cause them to dislodge eventually forming a fresh, young, atheroma. The new atheromas are very dangerous since they are unstable and can burst open. Well, guess what? CB2 stimulation seems to counteract this process by a mechanism as yet to be discovered. That’s remarkable news!
The dichotomy of the CB1 and CB2 receptor on endothelial function is similar to effects on macrophages, where CB1 agonism promotes a proatherogenic profile [increases plaque growth], and CB2 agonism prevents atherogenesis [decreases plaque].
I mentioned earlier in the article that CB1 blockage led to decreased inflammation. Now in these studies we see that stimulation of CB1 is pro-atherogenic (not good) while stimulation of CB2 decreases the inflammatory response in plaque formation (very good).
So it sounds as if a drug which blocks CB1 and stimulates CB2 may be a powerful tool for cardiac patients. Thus, the available evidence suggests a diverse role for CB1 and CB2 receptors in the progression of atherosclerosis and inflammation.
RIMONABANT-NOT
This led investigators to try Rimonabant, a CB1 antagonist, as a possible solution for decreasing plaque burden in human volunteers. In this study CB1 blockade was about as well received as a mendacious mother-in-law. After 30 months in the AUDITOR Trial which used Rimonabant a CB1 antagonist[ref]O’Leary DH et al. Effect of rimonabant on carotid intima-media thickness (CIMT) progression in patients with abdominal obesity and metabolic syndrome: the AUDITOR Trial. Heart. 2011 Jul;97(14):1143-50. Epub 2011 May 24.[/ref], it did not reduce plaque in the experimental group according to O’Leary the main author.
REPERFUSION INJURY AND THE ENDOCANNABINOID SYSTEM
Coronary and carotid arterial occlusion…after plaque rupture is the major cause of myocardial and cerebral infarction [stroke]. Together these acute events represent the leading cause of death worldwide. Early reperfusion is the best method to salvage the ischemic organ; however, it leads to additional damage known as reperfusion injury. …targeting the endocannabinoid system might evolve as a novel therapeutic concept to limit the devastating consequences of these acute vascular events through a wide variety of mechanisms, including lowering inflammation, oxidative stress, fibrosis, and excitotoxicity, and enhanced blood flow.[ref]Tuma RF, Steffens S. Current pharmaceutical biotechnology 13:1 2012 Jan pg 46-58[/ref]
The colossal damage that occurs from reperfusion injury during stroke, and heart attack is attenuated by blocking the pro-inflammatory CB1 receptor while stimulating the CB2 receptor leading to significant reductions in inflammation as seen below.
In this investigation it was demonstrated that CB1 activation promoted pro-inflammatory responses of macrophages through the production of reactive oxygen species. Blocking the CB1 receptor in conjunction with activation of the CB2 receptor suppressed the pro-inflammatory responses of the macrophages.[ref]Ronald F. Tuma et al. Targeting the Endocannabinod (sic) System to Limit Myocardial and Cerebral Ischemic and Reperfusion Injury. Current Pharmaceutical Biotechnology, 2012, 13, 46-58[/ref]
CB2 RECEPTORS PROTECT
In summary, the above studies suggest that blocking CB1 and stimulating CB2 decreases the inflammatory response. Furthermore, it appears that the CB2 receptor system is a protective arrangement in which IA’s like nicotine or oxidized fats, stimulate the proliferation of CB2 receptors which in turn limit the extent of inflammatory damage, as seen:
…under pathophysiological conditions such as inflammatory stimulation or tissue injury, increased CB2 receptor expression levels have been reported in the cardiovascular system, which probably reflects a protective response to limit cell or tissue injury (Pacher and Mechoulam, 2011). For example, up-regulation of CB2 receptor expression [increased number of receptors] has been described in primary human endothelial and smooth muscle cells stimulated by pro-inflammatory triggers and/or mitogens [IA’s] (Rajesh et al., 2007a; 2008; Ramirez et al., 2012), in human and mouse atherosclerotic plaques (Steffens et al., 2005), neointimal lesions following balloon injury (Molica et al., 2012) and in the myocardium of chronic heart failure patients (Weis et al., 2010).[ref] Sabine Steffens and Pal Pacher Targeting cannabinoid receptor CB2 in cardiovascular disorders: promises and controversies. Br J Pharmacol. Sep 2012; 167(2): 313–323. [/ref]
The authors Sabine Steffens and Pal Pacher (yes, that’s his real name) speculate that the CB2 signalling is part of a protective response against human plaque vulnerability, which is impaired in patients with acute heart attack or stroke.
In the final instalment of this series, we will discuss what lies outside of CB 1 & 2 receptor pharmacology and some of the properties of CBD a phytocannabinoid with some very interesting chattels. Lastly, we’ll discuss the results of one study that didn’t paint medical marijuana in a pretty light; and some of the exciting things that await us in the very near cannabis future.
You can read Parts 1 & 2 of Dr. Chris Rasmussen’s articles by clicking on the links below:
The Use of Cannabis as a Potent Anti-Inflammatory Medication - Part 2
The Use of Cannabis as a Potent Anti-Inflammatory Medication – Part 2
In part 1 of this article, some of the general applications of cannabinoids both synthetic and natural were covered. The power in these mysterious substances, comes at least in part, from their anti-inflammatory effects. In this article, we’ll cover the chronic immune response, where it lurks, the definition of cellular inflammation, and active areas of research where cannabis plays a special role.
Many would argue, myself included, that nearly all disease of affluence are inflammatory. Chronic inflammation is the bane of civilization. This is the response that we are trying desperately to decrease or eliminate among those that suffer from its torpor. The biggest problem is that, with few exceptions, it doesn’t respond well to our pharmaceuticals either. As a result we have an enormous number of people suffering from chronic, degenerative diseases for which there is no cure. It has been shown that cannabis reduces pain and inflammation under these circumstances.
This is one of the main reason why and how medical marijuana came to be legalized in certain states of America.
So what exactly is it that cannabis helps?
Let’s start first with a general definition so that we can all speak the same language. Chronic inflammation is an unchecked biological reaction to tissue injury producing a smoldering, cascade of immuno-vascular responses in an attempt to heal, leading to a pathologic change in the cell population of the affected tissue. It is characterized by repeated healing and injury.
Arterial plaque (and much more) is a result of the above response. Simply living La Vida Industria is all it takes sometimes. It is real tissue injury. Here I’m referring to atherosclerosis because of its textbook presentation, but we could just as easily be describing other pandemics like metabolic syndrome, neurodegeneration like Alzheimer’s disease, or chronic pain. In total there are three main regions where inflammation prefers to occur: blood vessel, brain and as an excess of visceral fat.
Let me saturate you in acronyms for a moment as we devil into the details. One of the 30 or so maligned products of visceral fat cells (belly fat as it is sometimes called), TNF-alpha, is a known cytokine (immune cell messenger) that activates NF-kB. This odd sounding chemical messenger is at the core of chronic inflammation.
The definition of cellular inflammation is increased activity of the gene transcription factor known as Nuclear Factor-kappaB (NF-kB). This is the gene transcription factor found in every cell, and it activates the inflammatory response of the innate immune system.[ref]Barry Sears PhD. What is Cellular Inflammation? (http://www.zonediagnostics.com/cellular-inflammation/) 08/06/2013[/ref]
CANCER
This immune response can be triggered by anything that stimulates the activity of NF-kB. It also paves the way for the third biggest killer in the western world – cancer.
The role of inflammation in evolution of certain types of cancer has been strongly suggested, linking the inflammatory response to 15–20% of all deaths from cancer worldwide….If genetic damage is the “match that lights the fire” of cancer, some types of inflammation may provide the “fuel that feeds the flames.”[ref]Lancet. 2001 Feb 17;357(9255):539-45.[/ref]
Cellular inflammation is the initiating cause of chronic disease because it disrupts hormonal signaling networks throughout the body.[ref]Barry Sears PhD. What is Cellular Inflammation? (http://www.zonediagnostics.com/cellular-inflammation/) 08/06/2013 p. 1[/ref]
TARGETING CELLULAR INFLAMMATION WITH CANNABIS
Unfortunately, for many with chronic, degenerative diseases in advanced stages we need bigger guns which we do not have. Patients with high levels of silent or overt inflammation (pain) are often left in the lurch. These are the patients I would see who have been through a dozen doctors, taking 20 or more medications, and are no better off.
Wouldn’t it be amazing if we had drugs that operated on the cellular level to help these patients? A drug or supplement that might suppress NF-kB?
Well, we already have some, but most are not commercially available yet. Can you say cannabinoids?
While there is a paucity of good anti-inflammatory prescription medications that a doctor can treat you with, current research demonstrates that several classes of cannabinoids can influence many of the inflammatory mechanisms mentioned above.
Let’s look at the classic model of inflammation once again: atherosclerosis.
CB1 BLOCKADE & CB2 STIMULATION DECREASE PLAQUE
It turns out that cannabinoids, acting via both CB1 and CB2 receptor modulation, have an important role in immune system regulation. Because inflammation plays a key role in atherogenesis, cannabinoids can potentially affect atherogenesis via modulation of the immune system[ref]Sandeep Singla MD. Cannabinoids and Atherosclerotic Coronary Heart Disease .Clinical Cardiology
Volume 35, Issue 6 pages 329–335, June 2012 (online: http://onlinelibrary.wiley.com/doi/10.1002/clc.21962/full) 11/23/2014[/ref]. CB1 & CB2 receptors have been identified on many immune cells and endothelial cells. Let’s see what the data shows:
Both CB1 and CB2 are G-protein coupled receptors that modulate second messengers and signalling components such as adenylate cyclase,…and members of the nuclear factor κ B (NF-κB) family. [ref]IBID[/ref]
In one study a synthetic cannabinoid agonist (stimulant) with CB2 selectivity was used. The decrease in extent of atherosclerosis was associated with a decrease in pro-inflammatory cytokine gene expression and attenuated oxidized low-density lipoprotein (ox-LDL)-induced NF-κB activation[ref]IBID[/ref].
In other words a synthetic CB2 stimulant (agonist) decreased plaque formation through a reduction in NF-kB.
What these studies suggest is that we may have a new, powerful, and potentially game-changing syllabus of cannabinoids that may actually “cure” heart disease, and by inference dozens of other chronic inflammatory diseases.
In part three more compelling evidence of the use of cannabis in suppressing inflammation will be provided.
You can read Part 1 of Dr. Christopher Rasmussen’s articles on Cannabis and Inflammation here.