Does Cannabis Impair Driving Ability?
Does Cannabis Impair Driving Ability?
If you surf over to the NIDA website Drugabuse.com they have this to say regarding weed and operating heavy equipment.
Does Cannabis Impair Driving Ability?
Marijuana significantly impairs judgment, motor coordination, and reaction time, and studies have found a direct relationship between blood THC concentration and impaired driving ability (Accid Anal Prev. 2010;42:859-866; Clin Chem. 2013;59:478-492). Marijuana is the illicit drug most frequently found in the blood of drivers who have been involved in accidents, including fatal ones (Am J Epidemiol. 2014;179(6):692-699; although it is important to note that marijuana can remain detectable in body fluids for days or even weeks after acute intoxication). A meta-analysis of multiple studies found that the risk of being involved in an accident roughly doubles after marijuana use (Drug Alcohol Depend. 2004;73:109-119).
Accident-involved drivers with THC in their blood, particularly higher levels, are three to seven times more likely to be responsible for the accident than drivers who had not used drugs or alcohol. The risk associated with marijuana in combination with alcohol appears to be greater than that for either drug by itself (Clin Chem. 2013;59:478-492).
Cannabis is unique among intoxicants because of its very long half-life. A half-life is the amount of time needed for half of the serum level of a drug to be removed from the body. The longer the half-life the longer it remains in your system.
Cannabis has a long half-life in humans (67 days). In chronic cannabis users, it is particularly difficult to determine whether a positive result for cannabis represents a new episode of drug use or continued excretion of residual drug. Algorithmic models have been devised to determine whether THC levels represent new use or the carry-over from previous use. However, these models are not very accurate in discriminating new use and carry-over in chronic users.[ref]Iran J Psychiatry. 2012 Fall; 7(4): 149–156.[/ref]
The above quote reminds us that when chronic cannabis users are tested for THC, a positive result can be from last week’s ingestion or from the same day. Therefore, even though marijuana is the most commonly found drug in motor vehicle accidents (MVA) it may be just along for the ride (pardon the pun). It may have nothing to do with the intoxicated state the driver was in at the time of the accident.
And from the 2014 NIDA study by Dr Volkow:
Immediate and long-term exposure to the substance [marijuana] has been found to substantially impair driving ability…
Some of the clarifications on the benefits and harms of cannabis come from the website[ref](http://clinicalcannabisincontext.tumblr.com/) 07/12/2015[/ref] of Ian Mitchell, MD, FRCP (Emergency Medicine staff Physician – Royal Inland Hospital Emergency Department and King Street Clinic, Kamloops, BC).
Lastly, although several recent studies have not been able to show any evidence of increased risk of traffic accidents due to the use of cannabis, the literature in totality suggests an overall doubling of risk. This is roughly equivalent to a BAC of less than 0.05. Driving with a BAC of 0.07, legal in many jurisdictions, is far more dangerous BAC of 0.07, especially for the younger driver.
The last sentence does not read well. His point is that a BAC of 0.07 is far worse for teenagers than the equivalent BAC of 0.05 that one would conceivably develop after smoking marijuana. In other words alcohol is still by far the main ingredient in your motor vehicle accident recipe.
Meanwhile, there does appear to be a synergy between pot and alcohol which makes it a bad idea should you elect to drive drunk and stoned. This is an important point for those who feel that cannabis has no untoward effects.
One can’t really argue these statistics. Pot is an intoxicant and you should never be driving while intoxicated. You just have to assign a drug-free friend or acquaintance to drive you to the nearest market for that gallon of ice cream you’re craving at 2 AM.
There clearly is a doubling of risk when driving after ingesting cannabis. Therefore, be careful and refrain from driving a car, or operating that front-end loader you recently purchased, if at all possible when high.
Cannabis and Increased Risk of Mental Illness
CANNABIS AND INCREASED RISK OF MENTAL ILLNESS
From the University of Warwick located in the heart of England, adjacent to the city of Coventry, a research team set out to examine whether cannabis consumption made patients manic or if mania symptoms preceded pot use. In 2015, they published their disturbing findings in the Journal of Affective Disorders.
Lead author Dr Steven Marwaha said: Previously it has been unclear whether cannabis use predates manic episodes. We wanted to answer two questions — does cannabis use lead to increased occurrence of mania symptoms or manic episodes in individuals with pre-existing bipolar disorder? But also, does cannabis use increase the risk of onset of mania symptoms in those without pre-existing bipolar disorder?[ref]Cannabis use and mania symptoms: A systematic review and meta-analysis. Journal of Affective Disorders, 2015; 171: 39[/ref]
After searching through the available data from previous studies the researchers concluded that marijuana use preceded the onset of mania symptoms. Not only that but cannabis smoking worsened pre-existing mania symptoms in patients already diagnosed with bipolar disorder.
The observed tendency for cannabis use to precede or coincide with rather than follow mania symptoms, and the more specific association between cannabis use and new onset manic symptoms, suggests potential causal influences from cannabis use to the development of mania. It is a significant link.
….our review suggests that cannabis use is a major clinical problem occurring early in the evolving course of bipolar disorder.[ref]IBID[/ref]
There is a lack of investigational studies on cannabis and mania or bipolar disorder suggesting that this is a relatively neglected area of research the author said.
What we do know is that the associations of mania and cannabis use are so significant that the study team suggested there is a strong possibility that something in marijuana causes or worsens mania symptoms. From another study released this year (2015) in the Journal of Affective Disorders:
Studies support an association between cannabis use and the exacerbation of manic symptoms in those with previously diagnosed bipolar disorder. Furthermore, a meta-analysis of two studies suggests that cannabis use is associated with an approximately 3-fold… increased risk for the new onset of manic symptoms.[ref]IBID[/ref]
CASE STUDY: ACUTE MANIA IN A 21 YEAR OLD MALE
Studies have also shown that cannabis is the most commonly abused drug among those diagnosed with bipolar disorder.[ref]Psychiatry (Edgmont). 2009 Dec; 6(12): 44–48. Published online 2009 Dec.[/ref]
What follows is the case of a college student who initially suffered from an acute psychotic breakdown secondary to cannabis use that later manifested into a permanent diagnosis of bipolar disorder with psychosis.
Mr. X is a 21-year-old, African-American man who was brought to the Greater Binghamton Health Center (GBHC), Binghamton, New York, for exhibiting hostile and grandiose behavior. This was his second psychiatric hospitalization. He was discharged one week prior after a 30-day stay with a diagnosis of cannabis-induced psychotic disorder. After being discharged and having no overt psychotic symptoms, he started using cannabis again and became symptomatic with more pronounced delusions and psychotic behavior.
What makes this case interesting and special is that he had no known risk factors for psychosis. He was highly functional prior to admission maintaining a 3.3 GPA with a major in chemistry. Yet he became psychotic apparently after simply smoking cannabis. His toxicology screen was positive only for marijuana. The authors comment:
Several case studies and longitudinal studies have illustrated the link between acute psychosis and mania associated with cannabis (three citations). The most prominent symptoms elicited are auditory hallucinations, paranoid feelings of being persecuted, depersonalization, derealization, anxiety, grandiosity, irritability (four citations). The debate remains as to whether or not cannabis can cause schizophrenia and bipolar disorder in an otherwise healthy individual.[ref]IBID[/ref]
Questions that need addressing are what formulations of marijuana tend to aggravate mania symptoms? Is it the THC content? What about the potential effects using strains high in CBD and very low in THC like Charlotte’s Web? Perhaps these varietals will help attenuate manic symptoms. What about using pure CBD administered sublingually?
There is nothing currently in the literature that can help shed light on these and other unknowns. In order to know for sure placebo controlled, randomized, double-blinded studies need to be organized using human volunteers.
Based on these and other findings I would suggest that young people be very, very cautious before using cannabis for the first time-especially if you have ANY family history of psychiatric disease. The risk for developing “affective” disorders in otherwise normal people with no risk factors for mania or psychosis is small but possibly real. Use caution until we know for sure what’s happening at a biochemical and clinical level.
Does Cannabis Significantly Impair Brain Function?
Does Cannabis Significantly Impair Brain Function?
How long does it take when discussing marijuana use before someone reminds you of the “facts” of cannabis? Your typical layperson (and some scientists) might mention things such as addiction, psychosis, and long-term cognitive dysfunction. While all of these “facts” are shouted from the spire as if they were established mathematical theorems, very little evidence exists which prove these assumptions.
The Daily Mail is one such place where vociferous weed whacking is the norm. They provide plenty of misinformation to those interested in supporting emotional arguments rather than scientific ones. Very often you’ll see articles featuring “reefer toking” brain-addled, hooligans on a robbing spree and whatnot.
As society braces for full legalization, detractors will be pouring from their hives reminding us that cannabis is not a harmless substance that simply makes you giggle and eat cupcakes. (Wait, it’s not?). In fact, they will tell you that marijuana is actually quite dangerous-even as a medicine.
But don’t become alarmed-not yet anyway. The facts speak differently when it comes to preserving brain function in chronic cannabis use.
YOUR CD PORTFOLIO
One such dangerous adverse effect is generating a lot of fog: cognitive dysfunction (CD). Sure sounds scary doesn’t it? What does the term mean when your cognition is defunct? How does it apply to cannabis smokers?
Recently, a meta-analysis (a study of many past studies) by Grant et al.[ref]J Int Neuropsychol Soc. 2003;9:679–89.[/ref] identified residual verbal memory impairments as the most consistent [cognitive dysfunction] deficit associated with chronic cannabis use in otherwise healthy users. Translated that means basically a decrease in short-term memory.
Below are two excerpts from a list of harms from a 2014 NIDA study. I will return to this study in another follow up article. These points cover other features of CD, or “cognitive dysfunction.”
In addition, adults who regularly smoked the substance during adolescence have impaired neural connectivity in areas that involve alertness, awareness, learning, and memory compared with those who have never smoked marijuana.
They also have less functional connectivity in areas that include processing habits and routines and inhibitory control, as well as a significant decline in IQ.
The references used from the above NIDA study was based on previous research which suggested that there were areas of the brain physically altered from cannabis use. These have been debunked by this most recent study:
No statistically significant differences were found between daily users and nonusers on volume or shape in the regions of interest. Effect sizes suggest that the failure to find differences was not due to a lack of statistical power, but rather was due to the lack of even a modest effect. In sum, the results indicate that, when carefully controlling for alcohol use, gender, age, and other variables, there is no association between marijuana use and standard volumetric or shape measurements of subcortical structures[ref]http://clinicalcannabisincontext.tumblr.com/. Original: (http://www.jneurosci.org/content/35/4/1505.abstract) 07/13/2015[/ref]
They were looking at physical variations in key subcortical brain structures to see if they were altered from cannabis use. They found no changes.
This study contradicts the facts from the NIDA publication above and renders it obsolete. It was a well-executed trial too. Based on this we conclude that chronic marijuana use does not permanently alter brain structure as previously thought.
8 "Facts" About Cannabis from the National Institute of Drug Abuse
8 “Facts” About Cannabis from the National Institute of Drug Abuse
A highly biased study was recently published (2014) in the New England Journal of Medicine titled Adverse Health Effects of Marijuana Use. It concluded that chronic marijuana use causes several serious consequences. This persnickety publication was written by author Dr. Nora D. Volkow, lead investigator, and director of the National Institute on Drug Abuse.[ref]N Engl J Med 2014; 370:2219-2227June 5, 2014[/ref]
Perhaps I’m naive but I think anyone working for NIDA would not be painting any “drugs of abuse” in a nice light even if they were proven harmless. Try to view this study as no more than a scientifically gilded opinion piece.
Much of the ammo used to bash marijuana hails from this publication and several others of the same ilk.
Let’s stroll through the major points of the study.
8 “Facts” About Cannabis
Their results included the following:
1. Approximately 9% of people who experiment with the substance will become addicted.
2. One in 6 of those who start using marijuana as teenagers will become addicted.
3. Cannabis withdrawal syndrome is real and can make cessation difficult.
4. Marijuana addiction increases the risk for using other illicit drugs.
5. In addition, adults who regularly smoked the substance during adolescence have impaired neural connectivity in areas that involve alertness, awareness, learning, and memory compared with those who have never smoked marijuana.
6. They also have less functional connectivity in areas that include processing habits and routines and inhibitory control, as well as a significant decline in IQ.
7. Regular use of cannabis has also been associated with an increased risk for depression and anxiety; it has been linked to psychoses (especially in those with a preexisting genetic vulnerability), and it exacerbates the illness in patients with schizophrenia.
8. Immediate and long-term exposure to the substance has been found to substantially impair driving ability. But studies on whether it contributes to lung cancer are unclear.
From the same article in the New England Journal of Medicine we have listed in the review highlights from Medscape.org which states:
Addiction to marijuana is a real phenomenon. Cannabis withdrawal syndrome is characterized by irritability, insomnia, dysphoria, and anxiety. Approximately 9% of individuals who experiment with marijuana will become addicted. However, this rate increases to 17% among people who began using marijuana during adolescence, and up to half of individuals who smoke marijuana daily are addicted.
Marijuana use during early adolescence is associated with worse school performance and a higher risk of dropping out of school.
Solid epidemiologic [associations again] evidence exists that marijuana acts as a gateway drug to the use of other, more harmful illicit drugs. Animal models suggest that THC, the main active ingredient of marijuana, can prime the brain for enhanced responses to other drugs.
Heavy marijuana use has been associated with unemployment, criminal behavior, lower income, and reduced satisfaction with life.
Marijuana is the most commonly cited illicit drug in promoting motor vehicle crashes. A meta-analysis found that using marijuana increased the risk for a motor vehicle crash approximately twofold. Other research has found that the risk for motor vehicle crashes after the use of marijuana is similar to that of persons beyond the usual legal limit of blood alcohol while driving.
Dear reader, wherever you see the term “associated” in the sentences above you should remember that there is no proof that marijuana does anything of the sort.
These studies by definition are weaker than randomized, double-blinded, placebo controlled clinical trials-the gold standard. As such they only suggest that there is a possibility that pot could be causing these problems but for proof we need the gold standard.
'CBD More Effective for Psychosis than Prescription Drugs', Dr. Christopher Rasmussen
‘CBD More Effective for Psychosis than Prescription Drugs’, Dr. Christopher Rasmussen
While THC rich strains of pot can potentiate an already psychotic or prepsychotic state, CBD alone or CBD rich stains of weed, actually behave as antipsychotics. Yes, you heard correctly. CBD is emerging as a potent antipsychotic medication as seen below.
In 2012 an elegant, randomized, double-blinded trial headed by doctors Leweke, and Piomelli in a joint effort covering both Europe and the US respectively, found that a novel phytocannabinoid found in marijuana called CBD behaved as well as a powerful antipsychotic medication.
CBD MORE EFFECTIVE FOR PSYCHOSIS THAN PRESCRIPTION DRUGS
Surprisingly, CBD was found to be as efficacious as the European blockbuster antipsychotic drug amisulpride which was used in the study. Amisulpride, an atypical antipsychotic, is not available in the US but has a similar profile to many of the drugs currently used in America. Amisulpride is one of the most effective drugs currently in use for the treatment of schizophrenia.[ref]Am J Psychiatry 2002; 159: 180–190.[/ref]
Can it get better? Indeed, CBD was found to be as good as the potent antipsychotic used in the study, plus it turns out that the side effect profile of CBD was decidedly superior when compared to amisulpride.
I’m not surprised. As mentioned previously, the antipsychotics are dangerous drugs with some of the worst adverse drug effects of any pharmacologic category. For example, chronic use of the antipsychotics increases a patient’s risk for Parkinson’s disease, or technically Parkinsonism (identical in form and function but due to the drug not true Parkinson’s disease). I don’t have the space to discuss it here but these pharmaceuticals have several other grave adverse effects. That’s a great reason to look for less toxic medications such as CBD.
In fact, when you list the side effects of CBD next to the side effects and adverse drug effects of amisulpride, you immediately notice something remarkable. There basically are no side effects with CBD usage. That may not seem very important to you but trust me, all pharmaceuticals have side effects and many are disasters waiting to happen. So a “drug” (CBD) as powerful as a pharmaceutical antipsychotic without the disaster waiting in the wings is truly amazing.
THE OLD THEORY
Clinical investigators historically have suggested that hyperactivity of the endocannabinoid system may contribute to the psychotic state. This theory was based on previous studies which showed that potent THC preparations and other cannabinoid agonists can induce psychosis in healthy and schizophrenic patients. We discussed some of this research in my Reefer Madness series.
This proposed model of madness fueled two large-scale clinical trials using CB1 cannabinoid antagonists (blockers) in schizophrenic patients. Sadly, the study failed to demonstrate any positive results. Thus sinking the hypothesis that an overactive endocannabinoid system makes one as mad as a hatter.
SOMETHING NEW
In a brilliant move, Dr Leweke and his team decided to test a diametrically opposite theory based in part on studies that showed schizophrenic patient’s symptoms correlated inversely with cerebral spinal fluid (CSF) anandamide levels. That is, the higher the patient’s brain anandamide levels the less intense their symptoms were. A shopping list of compelling data also implicated CBD as a player.
The author’s state:
Furthermore, preliminary clinical case reports suggest that cannabidiol might exert antipsychotic effects in schizophrenic patients (three citations). In addition, experimental studies show that cannabidiol reduces psychosis-like effects of Δ9-tetrahydrocannabinol and synthetic analogs (two citations).[ref]Translational Psychiatry (2012) 2, e94; doi:10.1038/tp.2012.15 Published online 20 March 2012[/ref]
A RIDE WITH ANANDAMIDE
Anandamide is the human body’s native THC-like neurotransmitter acting on CB receptors. It is responsible for the regulation of pain, mood, and cognition. Running point on this topic, studies showed that pharmacologic blockade of anandamide degradation (metabolism) attenuates rather than enhances psychotic behavior clinically and in an animal model.
In other words using CBD (at 800 mg per day) blocks the activity of the enzyme (called FAAH) that normally eliminates anandamide at the synapse within the recesses of the brain. Very quickly scientists noted that psychotic symptoms in patients decreased markedly. It acted like an atypical antipsychotic but its mechanism of action was through a vastly different and novel brain pathway.
Dr Leweke comments on his study conclusions:
Either treatment was safe and led to significant clinical improvement, but cannabidiol displayed a markedly superior side-effect profile. Moreover, cannabidiol treatment was accompanied by a significant increase in serum anandamide levels, which was significantly associated with clinical improvement. The results suggest that inhibition of anandamide deactivation may contribute to the antipsychotic effects of cannabidiol potentially representing a completely new mechanism in the treatment of schizophrenia.[ref]Translational Psychiatry (2012) 2, e94; doi:10.1038/tp.2012.15 Published online 20 March 2012[/ref]
ENTER CBD
In a previous publication I mentioned that CBD has numerous activities within the brain leading to complex end effects.
CBD itself is a weak, partial antagonist of CB1 receptors (THC is a weak agonist). Even though it weakly blocks CB1 receptors, its downstream effects appear to be the opposite of a blockade. That’s because CBD inhibits the enzyme responsible for the degradation of anandamide. That activity leads to an increase in the brain’s anandamide level which has a profound effect on the dampening of positive (voices) and negative (social withdrawal) aspects of madness. This feature plays a central role in our discussion of why CBD has such powerful antipsychotic activity.
Overall it appears that CBD’s effects are excitatory on the endocannabinoid system resulting in increased production of anandamide which is a very good thing for persons suffering from schizophrenia.
In concluding the author notes:
These results suggest that cannabidiol is as effective at improving psychotic symptoms as the standard antipsychotic amisulpride.
THIS SHOULD HAVE MADE HEADLINES
You didn’t read about this in the Times or USA Today but you should have. That’s because CBD is a natural compound and cannot be patented. Therefore, Big Pharma will not spend the time or money in its development. That means you will not see it promoted by the major news outlets. So we have to make sure patients know about this treatment all on our own.
I cannot emphasize enough on how important this finding is. What this study suggests is nothing short of a new paradigm in psychiatric research. It reveals that madness may have more to do with the recently discovered endocannabinoid system than with the classic model of insanity which predicates its theory on overexcited dopaminergic pathways in the brain.
Classically, the theory goes like this: madness has been viewed by the medical establishment as due to overactivity of dopamine (and several other neurotransmitters: serotonin being one of them) within special compartments in the central nervous system (CNS). Drugs which purportedly treat psychosis are designed to block dopamine (and serotonin with the atypicals). This helps to explain why the antipsychotics don’t work as well as they should. They may simply be active on the wrong system entirely.
The reason why this study is monu-“mental” is because number one, the antipsychotics both the classics (like Thorazine) and the atypicals (like amisulpride), provide more of a chemical lobotomy (Dr Peter Breggin Toxic Psychiatry); and number two, the antipsychotics are rife with a ledger of appalling side effects.
If further investigations prove CBD to be a prevailing antipsychotic it will usher in a golden age for psychiatry. It’s about time too. It will lift the specialty up and away from the medieval appurtenances it has so far relied upon. That’s of course if psychiatrists are willing to try a compound that will never be patented and will never appear in any of the glossy pages of their trade journals.
Dr. Rasmussen Explains the Truth About Cannabis and Schizophrenia
Dr. Rasmussen Explains the Truth About Cannabis and Schizophrenia
I’m sure that many of you have already heard the mantra hailing past the naysayer’s camp of commercial medicine that cannabis smoking will increase your risk for psychosis. It’s a frightening argument which provides much needed ordinance for those “thought leaders” in medicine that are opposed to the use of cannabis for treating disease or the legalization of it.
In fact, it’s one of the main batteries used to discourage patients from trying cannabis for intractable seizure disorders-those who suffer from status epilepticus- which I have previously exposed. Fair enough contention. But is there any evidence, real evidence, that this is a tangible and significant risk?
I always find it amusing that certain highly educated, yet mulish, physicians will look for any reason to avoid recommending pot. Reaching for straws, with arms akimbo, if they can find a hypothetical motive to support their obstinance, they will run with it-even if the threat is insignificant for healthy patients.
For example, based on a handful of suggestive trials some physicians would see your child worsen from a rare seizure disorder rather than expose the child to a greater risk for developing schizophrenia (S) or cognitive impairment later in life should the patient start using marijuana.
Our protagonists will assure you that schizophrenics (I’ll use psychosis and schizophrenia interchangeably) only use cannabis to help reduce symptoms of their disease. That they smoke cannabis because it helps them to deal with their impairment in a much better way.
In this series we will uncover the truth by examining the most recent research on this controversial subject. Here we’ll discuss the risk for psychosis in young, chronic pot smokers. As you will see the peril is real but very limited to a small subset: those “at risk.”
Let’s start with a definition of schizophrenia the model psychosis.
From the illustrious Mayo Brothers Clinic:
Schizophrenia is a severe brain disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behaviour.
Contrary to popular belief, schizophrenia isn’t a split personality or multiple personality. The word “schizophrenia” does mean “split mind,” but it refers to a disruption of the usual balance of emotions and thinking.
Schizophrenia is a chronic condition, requiring lifelong treatment.
The disorder generally manifests in late teens or early twenties, the “tweens.” There is a genetic component. Families with a schizophrenic parent have increased risk for children with this disease.
POTENT ANTI-PSYCHOTICS ARE NOT THE ANSWER
There is no known cure for schizophrenia. Patients are managed with powerful psychotropic medications, the classic and the atypical antipsychotics, for a lifetime. These medicines have proven to be a sword of Damocles for the unwashed masses given these drugs. The side effects are often at times so uncomfortable that some patients prefer suicide to a lifetime of being addled.
Moreover, these drugs promote heart disease and diabetes, stroke and heart attack. Class action suits have already been won. Therefore, in time, usually several decades, the patient often has a massive heart attack and often times it’s a “sudden death” event. I personally know of several people who have succumbed in this fashion. Then there are the devastating movement disorders that can occur with these drugs such as Parkinsonism and tardive dyskinesia. I bring this up because the sad state of psychiatry probably produces more illness than it helps.
You’ll hear both sides: that weed drives some users over the edge; or that pot acts as an antipsychotic. Referring to the latter, is there something in marijuana that helps schizophrenics deal with their disease? Perhaps with cannabis, traditional medications could be reduced or eliminated. Later on I’ll show you that indeed some cannabinoids may be the next “it girl” for treating schizophrenia.
THE POWERFUL ASSOCIATION WITH CANNABIS AND SCHIZOPHRENIA
A Times of London report stated that there are 210,000 people in the UK who suffer from schizophrenia, and a significant number of doctors feel that cannabis “caused” their condition.
Some of Britain’s most senior psychiatrists say the drug is now the “No 1 problem” facing mental health services. Psychiatrists in inner-city areas speak of cannabis being a factor in up to 80 per cent of schizophrenia cases, and mental health specialists are bracing themselves for an increase in the problem as reclassification is misinterpreted as an assurance that the drug is safe.[ref](http://www.schizophrenia.com/research/cannabis.htm) 07/06/2015[/ref]
Previously most authorities assured us that the use of cannabis among pre-psychotic patients with behavioral disorders was an attempt to self-medicate in the same fashion as one might use alcohol to help extinguish the anguish of psychosis.
In this segment we’ll uncover a disturbing, and often quoted, study which suggested that pot smoking caused a 300% increase in psychosis among that group. We’ll go over the significance of these findings and what they mean for the casual smoker of boutique buds and heady hashish.
Although most young people use cannabis without harm, a vulnerable minority experience harmful outcomes. A tenth of the cannabis users by age 15 in our sample developed schizophreniform disorder by age 26 compared with 3 per cent of the remaining cohort. Our findings suggest that cannabis use among psychologically vulnerable adolescents should be strongly discouraged by parents, teachers, and health practitioners. Policy makers and lawmakers should concentrate on delaying onset of cannabis use.I would say this is now the No 1 problem facing the mental health services in inner cities. In south London the incidence of psychosis has doubled since 1964.[ref]IBID[/ref]
From the above quote the term incidence means the number of new cases per a population, usually 100,000 people. There are at least 4 other studies that demonstrate the use of cannabis increases the risk for psychosis.
EPIDEMIOLOGY
Now let me clarify something tucked inside the observations discussed in the above study. These are epidemiologic studies. They can only show an association not a causation for disease. Therefore, a casual glance shows a clear association with cannabis and mental illness. But can marijuana actually cause a user to become psychotic?
What seems to be occurring here is that kids with a predisposition toward mental illness, such as having a family member with schizophrenia, who smoke cannabis increase their chances for a psychotic break. Under these unusual circumstances marijuana behaves more like a trigger unmasking an already budding psychosis. For these “pre-psychotics” it’s not if but when they break so to speak. Cannabis seems to hasten the process.
That budding psychosis in the last study was called schizophreniform disease or “schizophrenia light.” But does marijuana actually cause this in patients not normally predisposed to the development of psychosis? In other words, can it make you psychotic even if you have no risk factors for it?
Not likely. Based on four large-scale, peer-reviewed studies previously conducted, scientists have concluded that there was a strong link between schizophrenia and cannabis consumption with a dark horse emerging from the scientific literature. From an LA Times article:
Data from four such studies suggest that cannabis use doubles the likelihood of developing a psychotic illness later in life.
But a few small studies have flipped the direction of causation, suggesting that a genetic predisposition to schizophrenia…is itself a risk factor for smoking pot. That might explain why pot use is perennially high (pardon the pun) among those diagnosed with schizophrenia.[ref](http://www.latimes.com/science/sciencenow/la-sci-sn-schizophrenia-marijuana-20140624-story.html) 07/06/2015[/ref]
GENETIC LINK FOUND IN SCHIZOPHRENIC PATIENTS
A research team led by Robert Power, a psychiatry researcher at Kings College, published a most interesting study online in Molecular Psychiatry.
Their goal was to find important genetic links between schizophrenia and marijuana abuse.
We know that cannabis increases the risk of schizophrenia, lead author Robert Power, a psychiatry researcher at Kings College, said in a statement. Our study certainly does not rule this out, but it suggests that there is likely to be an association in the other direction as — that a predisposition to schizophrenia also increases your likelihood of cannabis use.[ref](http://www.schizophrenia.com/research/cannabis.htm) 07/06/2015[/ref]
LA Times author Geoffrey Mohan quips:
They analyzed the participants’ genome, looking for known variations that have been associated with schizophrenia. They found that those with the strongest genetic profile for schizophrenia risk also were more likely to use cannabis, and to use it in greater quantities.
Madness, they suggest, may lead to reefer.
Did you catch that? A most fascinating conclusion: it suggests that cravings for cannabis and a marker for susceptibility to schizophrenia are located in the exact same region of your genome. I’m certain no one saw that coming. In other words those people most likely to develop schizophrenia are also genetically most likely to abuse marijuana.
A new study from the Harvard School of Medicine was published in Schizophrenia Research titled A controlled family study of cannabis users with and without psychosis.
So researchers from Harvard Medical School and the VA Boston Healthcare system got together to determine whether family risk for schizophrenia is a crucial factor underlying the association between the development of schizophrenia in teens who smoke marijuana.
The researchers recruited 282 subjects from the New York and Boston metropolitan areas who were divided into four groups: controls with no lifetime history of psychotic illness, cannabis, or any other drug use; controls with no lifetime history of psychotic illness, and a history of heavy cannabis use during adolescence, but no other drug use; patients with no lifetime history of cannabis use or any other drug and less than 10 years of being ill; patients with a history of heavy cannabis use and no other drug use during adolescence and prior to the onset of psychosis.[ref](http://psychcentral.com/news/2013/12/10/harvard-marijuana-doesnt-cause-schizophrenia/63148.html) 07/06/2015[/ref]
They concluded that:
The results of the current study suggest that having an increased familial…risk for schizophrenia may be the underlying basis for schizophrenia in cannabis users and not cannabis use by itself.[ref]Proal, Ashley C. et al. A controlled family study of cannabis users with and without psychosis. Schizophrenia Research , Volume 152 , Issue 1 , 283 – 288[/ref]
The above study also found a tendency for depression and bipolar disorder to be increased in cannabis users in both the patient and control samples. This finding implies that cannabis users are more prone to affective disorders than their non-using samples or vice versa.
However, only future research will be able to unravel this curious relationship.
Meanwhile, a group from the University of Manchester published their findings in 2014 which did not find marijuana aggravated or in any way influenced psychotic behavior. Like the above study, cannabis was associated more with depression/anxiety in the high-use group. I quote:
There was no evidence of a specific association between cannabis use and positive symptoms [voices], or negative symptoms [withdrawal], relapse or hospital admissions. However, a greater dose of cannabis was associated with subsequent higher depression and anxiety. Change in the amount of cannabis used was associated with statistically significant corresponding change in anxiety scores, but not depression. Additionally, reductions in cannabis exposure were related to improved patient functioning. Conclusions: Reducing cannabis may be directly associated with improvements in anxiety and functioning, but not other specific symptoms, [such as psychotic behavior].[ref]Schizophr Bull (2014) doi: 10.1093/schbul/sbu095 First published online: July 9, 2014[/ref]
Note the use of the word association in the above description. Once again even the “affective” disorders amongst marijuana users correlate well but we still cannot conclude that pot use causes these other problems any more than it causes schizophrenia.
To clarify the issues involved regarding psychosis and cannabis use we must make sure that the data does not lead us down the wrong path. To wit there are scores of damning epidemiologic studies showing how cannabis smokers have a greater chance of developing multiple drug addictions, cognitive impairment, cancer, psychosis, anxiety, depression, and of course let’s not forget bronchitis to name a few. Many of these findings are from epidemiologic studies.
Remember that none of these epidemiologic observations proves the point; these studies only show associations. To prove something we need double-blinded trials that control for all variables. Yet, unfortunately, for that to occur we need marijuana to be removed from its schedule one status so that human volunteers can receive pot legally for study. That’s one of the fixes we are currently in, and it’s the main reason why so much information within this field is confusing.
These studies are still significant and worthwhile but they must be interpreted in the proper context. No matter how impressive an association is within a population it remains to be seen if that association is actually a causation. From the CDCs website:
Epidemiology is the study of the distribution and determinants of health-related states or events in specified populations, and the application of this study to the control of health problems.
Study
Epidemiology is a scientific discipline with sound methods of scientific inquiry at its foundation. Epidemiology is data-driven and relies on a systematic and unbiased approach to the collection, analysis, and interpretation of data. Basic epidemiologic methods tend to rely on careful observation and use of valid comparison groups to assess whether what was observed, such as the number of cases of disease in a particular area during a particular time period or the frequency of an exposure among persons with disease, differs from what might be expected. However, epidemiology also draws on methods from other scientific fields, including biostatistics and informatics, with biologic, economic, social, and behavioral sciences.
In fact, epidemiology is often described as the basic science of public health, and for good reason.
Epidemiology is also a statistician’s dream since the data can be manipulated to fit whatever theory one might be prejudiced with.
For example, let’s say an author of an observational study wants you to believe that TV causes heart disease. In his study he concluded that those who watch TV for more than four hours per day had a 50% increase in the risk for a heart attack.
OK fine, but other things to think about are the other slovenly habits these people have that may predispose them toward heart attacks. Perhaps TV watchers also eat junk food on a daily basis or maybe a greater percentage smoke cigarettes. Perhaps they don’t exercise. That’s why it’s important to understand that these epidemiologic studies in and of themselves say nothing that couldn’t be overturned with more rigorous trials.
However, it may turn out that cannabis does cause an increase in psychosis in those without a predisposition. It does not seem likely however based on what we know so far.
Let’s look at a different example: the proof that cigarette smoking caused lung cancer was initially discovered when epidemiologists noticed a much higher ASSOCIATION among tobacco users and lung cancer. The alarming number of cancers within all smoking populations were first noticed through epidemiologic investigations. That was followed with double-blinded studies to prove that is was an actual causation: that cigarettes caused lung cancer. That is now an accepted fact.
Same thing with the epidemiology of marijuana users and mental illness. We notice an increase in psychosis among users but the percentages are much smaller than the numbers of lung cancer patients seen in the above example, and the associations are much weaker.
For now all of the bad press with cannabis “causing” psychosis reflects simple epidemiological findings and nothing else.
Dr Deepak Cyril D’Souza sums it up:
It is likely that cannabis exposure is a “component cause” that interacts with other factors to “cause” schizophrenia or a psychotic disorder, but is neither necessary nor sufficient to do so alone.[ref]Eur Arch Psychiatry Clin Neurosci. 2009 Oct; 259(7): 413–431. Published online 2009 Jul 16.[/ref]
What are these other factors? What are the component parts?
For that, you guessed it, we need formal randomized, double blinded trials. Don’t hold your breath waiting as it may be years before the DEA grants easy access to cannabis for research. Based on what I have seen it takes about 6 years of red tape surfing before a research team gets their own legal marijuana for study.
That my good friends, is far too long.
How to Treat Anxiety Disorder with Cannabis
How to Treat Anxiety Disorder with Cannabis
Wait, say what? “I thought pot smoking gave you anxiety?” quipped the well-read observer.
Well, it sure can but what exactly is anxiety?
ANXIETY
From WebMD:
There are several types of anxiety disorders including panic disorder, social anxiety disorder, specific phobias, and generalized anxiety disorder.
Anxiety is a normal human emotion that everyone experiences at times. Many people feel anxious, or nervous, when faced with a problem at work, before taking a test, or making an important decision. Anxiety disorders, however, are different. They can cause such distress that it interferes with a person’s ability to lead a normal life.
An anxiety disorder is a serious mental illness. For people with anxiety disorders, worry and fear are constant and overwhelming, and can be crippling.
Yes, indeed some sensitive folks do become a little besmirched when ingesting cannabis. You hear about it all the time. Just recently a dear friend of mine I’ve known for years reported a serious, if not hilarious, episode of “anxiety,” after smoking a potent sativa strain called Jack Herer. Living in California she is allowed to use medical marijuana for her anxious condition.
“I wound up staying up most of the night baking pies, and woke up on the floor spooning a huge stuffed elephant. Now I’m sweating…at the pool with a weed hangover.”
Ok, so maybe this person needs to rethink marijuana as her “go to” anxiety medicine. Or maybe she needs to try an indica for its sleepier profile.
THE LIST
Here’s a list of some medicines that you could experiment with that are valued for their supposed positive applications in treating anxiety. There are strains that are high in CBD that may be just what you are looking for. Others still have THC in them but are famous for their sedative qualities.
Granddaddy Purple is one to consider.
Many people prefer indicas over sativas because they relax the mind rather than supercharge it. For this reason we recommend Granddaddy Purple, which eases you into a peaceful mindset while urging your body to release all that stress and tension.[ref](https://www.leafly.com/indica/granddaddy-purple) 06/17/2015[/ref]
Jack Herer is one recommended for some but not for our intrepid aforementioned patient. That much we can be certain of so approach this one cautiously.
A high-THC sativa typically wouldn’t be our first recommendation for anxiety; they tend to have racy cerebral effects that tug at anxiety rather than help it. But Jack Herer is different in that its euphoria tapers in gently with calming effects that could possibly be explained by Jack’s relaxing parent, Northern Lights.[ref](https://www.leafly.com/sativa/jack-herer) 06/17/2015[/ref]
Next we have Cannatonic.
For the THC-sensitive, we recommend the high-CBD hybrid Cannatonic. This strain typically has a CBD profile that sizes up to its THC content in a 1:1 ratio, which helps blunt the anxious edge that a lot of anxiety-sufferers experience with cannabis. Cannatonic tends to also boast high levels of the terpene myrcene which contributes to this strain’s deeply relaxing attributes.[ref](https://www.leafly.com/hybrid/cannatonic) 06/17/2015[/ref]
In general, when using concentrates for treating disease, they recommend the indica strains to induce a calm, sleepy patient which helps in healing the body of a dreadful disorder. There are some highly recommended indicas that are very good at treating insomnia. They are also good choices in relieving anxiety.
These would include Blackberry Kush known for its relaxed, sleepy effects.
Blackberry Kush is a heavy indica strain that inherits crushingly sedating effects from its Afghani parent and a sweet berry flavor from Blueberry. This may not be a strain you can indulge in throughout the day, but you’ll be more than grateful to have it at your bedside when insomnia rears its ugly head.[ref](https://www.leafly.com/indica/blackberry-kush) 06/17/2015[/ref]
Lastly there’s Purple Urkle.
Another powerfully relaxing indica strain, Purple Urkle annihilates the anxiety and stress that keeps you tossing and turning throughout the night.[ref](https://www.leafly.com/indica/purple-urkle) 06/17/2015[/ref]
I personally feel that sticking to the potent indicas is a better approach in treating the different manifestations of anxiety. But you be the judge of that. Let us know if any other strains are of particular importance in calming and relieving the symptoms of anxiety.
Cannabis Fights Neurodegenerative Disorders, as Explained by Dr. Rasmussen
Cannabis Fights Neurodegenerative Disorders, as Explained by Dr. Rasmussen
While examining the pro-pot and cannabis-cons from the World Congress on Pain, a certain expert physician quipped that one of the biggest drawbacks to recommending cannabis was that it causes neurodegeneration with chronic use.
Well, where’s the evidence?
I’m not convinced that he’s right. I have seen plenty of research showing that the cannabinoids actually protect the brain from neurodegeneration.
Technically, you can’t have both so which is it? Do the noble nuggets cause your brain to atrophy or do they protect you?
Not only is this appropriate to understand when concerned with neurodegenerative diseases, but also the average cannabis smoker needs to know if a marijuana habit will cause problems later in life.
Let’s start off on page one with a definition of neurodegeneration.
….in the strict sense of the word, neurodegeneration corresponds to any pathological condition primarily affecting neurons. In practice, neurodegenerative diseases represent a large group of neurological disorders…; they arise for unknown reasons and progress in a relentless manner. Conversely, neoplasm, edema, hemorrhage, and trauma of the nervous system, which are not primary neuronal diseases, are not considered to be neurodegenerative disorders. Diseases of the nervous system that implicate not neurons per se but rather their attributes, such as the myelin sheath as seen in multiple sclerosis, are not neurodegenerative disorders either, nor are pathologies in which neurons die as the result of a known cause such as hypoxia, poison, metabolic defects, or infections.
Among the hundreds of different neurodegenerative disorders, so far the lion’s share of attention has been given only to a handful, including Alzheimer disease (AD), Parkinson disease (PD), Huntington disease (HD), and amyotrophic lateral sclerosis (ALS). Many of the less common or publicized neurodegenerative disorders, though no less devastating, have remained essentially ignored.[ref]J Clin Invest. 2003 Jan 1; 111(1): 3–10.[/ref]
ENDOCANNABINOID PATHWAYS
Our growing understanding of the roles of the endogenous cannabinoids has suggested two main pathways by which cannabinoids may impact upon neurodegenerative processes; neuromodulation and immunomodulation.
Aside from this crucial regulatory role in the activity of neurons, endocannabinoids also play a key role in peripheral and brain immune function. As mentioned, CB2 is expressed on various circulating and resident immune cells, particularly when these cells are activated, and its agonism [stimulation] is typically associated with a dampening of their pro-inflammatory activities.[ref]Br J Pharmacol. 2010 Jun; 160(3): 480–498.[/ref]
DYSREGULATION OR ENDOCANNABINOIDS
Preliminary evidence suggests that regions of endocannabinoid hypofunction or dysregulation within the brain may be responsible for some of the symptomatology of a diverse group of neurodegenerative diseases including multiple sclerosis (yes, some authors list MS in the neurodegenerative category), Huntington’s (HD), Parkinson’s (PD) and Alzheimer’s (AD) diseases, and amyotrophic lateral sclerosis (ALS).
It’s also more than inquisitive that the abundance of CB1 receptors are bundled within singular areas of the brain responsible for executive thought and movement. Both of these regions are ground zero for degenerative movement disorders such as Huntington’s and Parkinson’s diseases.
This also provides a model for how cannabinoids may play a role in psychotic behavior. Psychosis is reputed to be due to overstimulation of dopamine pathways which are shared with CB receptors.
In HD, AD, and ALS we see upregulation (increase in the number) of CB2 receptors within the brain. This is a protective response which helps to mitigate the immune/inflammatory response that characterizes these diseases. Sadly, it is insufficient to prevent neuronal damage which may also be potentiated by the downregulation of CB1 receptors seen in HD and AD.
In MS, cannabinoids have shown great promise in animal models. Sativex®, an oromucosal spray composed of THC and CBD, has demonstrated efficacy in the treatment of spasm, neuropathic pain, and sleep disturbances seen in MS patients. It is approved by the FDA for this condition.
If the exciting findings of cannabinoid-mediated attenuation of inflammation, stimulation of remyelination [repair of certain neurons], and behavioural and symptomatic recovery translate from model systems to humans, cannabinoids may be promising therapeutics in MS.[ref]IBID[/ref]
In all of the disorders: ALS, MS, PD, and AD, it is uncertain if the alterations in endocannabinoids in these diverse diseases is a result of the cell destruction from the disease process itself. Or do the endocannabinoid changes cause the eventual development of these diseases?
In other words is the dysfunction of the endocannabinoid system in these ailments creating a condition ripe for neurodegeneration, or are these changes simply an artifact of extensive neuronal damage?
Whether integral to the disease, or a symptom of it, the studies described in this review highlight the potential role that endocannabinoids may play in either protecting cells from the disease process, or treating the symptoms of the disease.[ref]Br J Pharmacol. 2010 Jun; 160(3): 480–498.[/ref]
From MedicineNet.com:
Parkinson’s disease: A slowly progressive neurologic disease that is characterized by a fixed inexpressive face, tremor at rest, slowing of voluntary movements, gait with short accelerating steps, peculiar posture and muscle weakness (caused by degeneration of an area of the brain called the basal ganglia), and low production of the neurotransmitter dopamine. Most patients are over 50, but at least 10 percent are under 40. Treatment involves use of medication, such as levodopa and carbidopa.
This disease occurs from the cumulative destruction of dopaminergic neurons in an area of the brain called the nigro-striatal pathway.
Here the neuromodulatory effects of the endocannabinoids exist in tandem with dopamine pathways where there exists reciprocal regulation between dopamine and endocannabinoids.
For example D1 and D2 receptors (dopamine receptors within the brain) exist with CB1 receptors, called co-localization, on these neurons.
This arrangement leads to very complex signaling within this special area of the brain. So we know that endocannabinoids play a vital role, which type of role is not presently known in any detail.
THE WAY IS UNCLEAR
It’s too early to tell whether marijuana will be helpful in treating Parkinson’s disease. In PD patients, the endocannabinoid changes are difficult to assess. Due to the numerous pharmaceuticals PD patients need to take, researchers are hamstrung in teasing out what brain effects are due to the drugs and which are due to the disease.
Furthermore, it’s uncertain what the effect of powerful centrally acting medications, the so-called antipsychotics, have on the brain’s endocannabinoids. Only one study (Pisani et al., 2005) has assessed cannabinoid levels (AEA) within the brain. They found them to be double that of controls.
Studies on the potential therapeutic utility of cannabinoid agonists and antagonists in PD have also produced conflicting results. Some animal studies have shown promise while others have not.
The same is true for human studies where nabilone, a cannabinoid agonist, significantly reduced movement disorders in a special class of PD patients (Sieradzan et al., 2001) while cannabis had no effect on a group of PD patients in another study (Carroll et al., 2004).
ALZHEIMER’S DISEASE (AD)
Scientists have pondered a role for the cannabinoids in the development of AD since one of the first changes to occur is the loss of memory in early stage AD. Likewise, the loss of short term memory is legion among cannabis smokers.
From Alzheimer’s Foundation of America:
– Alzheimer’s disease is a progressive, degenerative disorder that attacks the brain’s nerve cells, or neurons, resulting in loss of memory, thinking and language skills, and behavioral changes.
– These neurons, which produce the brain chemical, or neurotransmitter, acetylcholine, break connections with other nerve cells and ultimately die. For example, short-term memory fails when Alzheimer’s disease first destroys nerve cells in the hippocampus, and language skills and judgment decline when neurons die in the cerebral cortex.
– Two types of abnormal lesions clog the brains of individuals with Alzheimer’s disease: Beta-amyloid plaques—sticky clumps of protein fragments and cellular material that form outside and around neurons; and neurofibrillary tangles—insoluble twisted fibers composed largely of the protein tau that build up inside nerve cells. Although these structures are hallmarks of the disease, scientists are unclear whether they cause it or a byproduct of it.
– Alzheimer’s disease is the most common cause of dementia, or loss of intellectual function, among people aged 65 and older.
– Alzheimer’s disease is not a normal part of aging.
THE WELL-KNOWN EFFECTS OF ALZHEIMERS ON MEMORY MAY BE RELATED TO ENDOCANNABINOIDS
The disruptive effects of Δ9-THC on memory are well documented and have recently been more fully characterized at the molecular level (Puighermanal et al., 2009). Alzheimer’s disease (AD), a disease with major impact on memory systems, has therefore been investigated for evidence of dysfunction of the endocannabinoid system resulting from, or contributing to, disease pathophysiology. AD is the most common neurodegenerative disorder, with a prevalence of approximately 10% in humans over 80 years old (Ferri et al., 2005).[ref]Br J Pharmacol. 2010 Jun; 160(3): 480–498.[/ref]
The rate of AD in an 85-year-old American is 50%, and it’s increasing. It eclipses all other forms of dementia by a long shot.
The brain’s microglia are special immune cells. In AD patients, researchers have discovered that CB2 receptors are expressed on the microglia clustered around beta-amyloid plaques. These plaques are pathognomonic for the lesions that develop in AD. It therefore suggests that endocannabinoids may have the ability to modulate the effector cells of AD (Benito et al., 2003)
While CB2 receptors are upregulated on microglia, scientists have unexpectedly discovered that CB1 receptors are decreased or downregulated. This is an unusual and unexpected finding. Note also that CB2 receptors are infrequently found centrally (in the brain). They are clustered more in the immune system and peripheral nervous tissues.
CANNABINOIDS AS THERAPEUTIC AGENTS IN ALZHEIMERS
Groundbreaking work over the last two decades suggests that cannabinoid agonists may play a therapeutic role in the treatment of AD.
Synthetic Δ9-THC (dronabinol) has been shown to alleviate behavioural disturbances and weight loss, and night-time agitation symptoms in human studies of Alzheimer’s and severe dementia respectively (Volicer et al., 1997; Walther et al., 2006).[ref]IBID[/ref]
Scientists have speculated on a unifying hypothesis for AD. In its broadest application it applies to other forms of neurodegeneration too. It states that pathologic changes in endocannabinoid levels within the affected regions of brain tissue, and CB2 expression, are induced by the inflammatory effects of the disease. In this case we are referring to AD. Therefore AD comes first, the endocannabinoid changes occur in response to the disease.
It’s a gallant attempt to heal dysfunctional brain cells. By increasing the quantity of CB2 receptors on the affected neurons the brain is partially able to decrease microglial activation. This activation, although well intended, is a powerful immune/inflammatory response which is responsible for much of the cellular damage seen in AD. It can be very destructive. AIDS related dementia is due to the same mechanism.
However, it’s too little too late. The upregulation of CB2 is insufficient to arrest the inflammatory damage to the neurons. The unexplained downregulation of CB1 receptors may potentiate this effect.
It appears then that the system suffers from a relative deficiency of endocannabinoids. The proof is that cannabinoid agonists help this situation by providing much needed stimulation of CB2 (and CB1) receptors.
On the basis of the pre-clinical efficacy already demonstrated, cannabinoid stimulators may have therapeutic benefit by augmenting the brain’s innate response.
Cannabinoid agonists in human trials to date have been well tolerated and safe, but clearly psychoactivity following CB1 activation is often an unacceptable consequence, particularly for long-term drug treatment; it is hoped that modulation of endocannabinoid levels may provide a more suitable alternative.[ref]IBID[/ref]
Although I agree in principle with the author’s last statement it should be noted that with chronic use the psychoactive effects of THC diminish over time. I don’t think the central effects of THC are as detrimental as many authors seem to suggest.
Let’s face it, some patients might even enjoy it.
The Efficacy of Cannabis on Seizures, As Explained by Dr. Rasmussen
The Efficacy of Cannabis on Seizures, As Explained by Dr. Rasmussen
One of the most frightening, life-threatening events that can occur in susceptible patients is developing a seizure that conventional medications cannot prevent or break. It’s called status epilepticus.
Here’s the main problem. During a seizure there is uncontrolled firing of neurons in parts of the brain or globally. During this period of increased brain activity, the involved neurons use a tremendous amount of oxygen. Within minutes the brain can become hypoxic (without oxygen) if the person cannot move air effectively because of the seizure. In a very short time (about three minutes of hypoxia), irreversible brain damage can occur should the seizure continue unabated.
This is truly a medical nightmare for both patient and physician.
STATUS EPILEPTICUS DEFINED
From E Medicine:
Status epilepticus (SE) is a common, life-threatening neurologic disorder that is essentially an acute, prolonged epileptic crisis.. SE can represent an exacerbation of a preexisting seizure disorder, the initial manifestation of a seizure disorder, or an insult other than a seizure disorder. In patients with known epilepsy, the most common cause is a change in medication. Most seizures terminate spontaneously
Pharmacotherapy
Most patients with status epilepticus who are treated aggressively with a benzodiazepine, fosphenytoin, and/or phenobarbital experience complete cessation of their seizures. If status epilepticus does not stop, general anesthesia is indicated.
Medications used in the treatment of status epilepticus include the following:
• Benzodiazepines (eg, lorazepam, diazepam, midazolam): First-line agents
• Anticonvulsant agents (eg, phenytoin, fosphenytoin)
• Barbiturates (eg, phenobarbital, pentobarbital)
• Anesthetics (eg, propofol)[ref](http://emedicine.medscape.com/article/1164462-overview) 06/21/2015[/ref]
In case you missed it the ultimate treatment for this life-threatening condition, when all else fails, is to go under anesthesia as if you were having surgery. That’s because general anesthetics are the most powerful drugs we have to “slow down” brain activity. This is performed to save the brain from hypoxia and to arrest the seizure.
As an anaesthesiologist I have never seen a case go this far but it is done often enough. Yet, it’s as if we need a jackhammer to kill a fly, even if the fly weighs two pounds.
All of the drugs we use for seizure disorders read like a who’s who of drug adverse effects. Perhaps one of the worst, and most familiar, is gingival hyperplasia from phenytoin use. You can recognize an adolescent chronically on phenytoin by their gums which tend to grow right over their teeth.
Yet, doctors who question the use of medical marijuana still reject it claiming they do not know enough of the safety profile of cannabis. That’s said with a straight face. Scientists still languish over “hypothetical harms” in spite of the fact that much of the planet uses the plant regularly, and have been for millennia, without much fanfare.
Meanwhile, to the amazement of people everywhere, a certain preparation of cannabis made national headlines last year. An extract from a strain called Charlotte’s Web was able to dispatch a “status” patients’ seizure with no more effort than it takes to fall off your roof.
Considering the big guns we sometimes need to control seizures, and the risks they entail, this news is very comforting.
I have a friend whose daughter was having dozens of seizures throughout the day. It went on for at least a year before being discovered. These are the type often missed except by the astute teacher with the eye of an Accipiter. Often called absence seizures or the old term petite mal. She was put on three antiseizure medications with little effect. Lucky for her, this was a condition that she eventually outgrew. Not so fluky for many others who must deal with relentless debilitating seizures.
PATHWAY OPENED FOR CLINICAL TRIALS
The US Food and Drug Administration (FDA) has given approval for studies to begin on a medicinal form of marijuana for the treatment of intractable epilepsy in children.
The drug, cannabidiol (Epidiolex, GW Pharmaceuticals) is the largest nonpsychoactive component of the cannabis plant. The product has also been granted orphan drug status for the treatment of children with Dravet syndrome, a rare and severe syndrome of infantile-onset, genetic, drug-resistant epilepsy.
Medscape Medical News reported an interview with lead author Dr Orrin Devinsky, of New York University School of Medicine. He mentions that this is the first formal study of CBD. The study was inspired by anecdotal reports of “miraculous” benefits using high CBD medicines for intractable seizure disorders or severe epilepsy.
THE AMERICAN EPILEPSY SOCIETY
Recently, a report was issued at the 68th annual meeting of the American Epilepsy Society (AES). After a lengthy review of case reports, open-label trials and informal surveys, they concluded that cannabis extracts high in CBD can be an effective adjunct to traditional medications.
This appears especially true for children with relatively rare disorders, such as infantile spasms, Lennox-Gastaut syndrome (LGS) and Dravet syndrome. And these products appear to be well tolerated.[ref](http://www.medscape.com/viewarticle/837487) 06/22/2015[/ref]
At the meeting, study researcher Dr Shaun Hussain, a pediatric neurologist at UCLA Medical Center, reported the results of an anonymous, online survey of parents treating their children’s seizure disorder with CBD. They had a total of 117 respondents who administered CBD extracts to their kids for an average of nearly 7 months.
Appallingly, over half of the parents surveyed could NOT accurately tell how much CBD their child was getting per day. The better-informed parents reported that each child was receiving on average about 4 mg/kg CBD per day. As such, a 40 kg child would be getting about 160 mg CBD per day. This dose was considerably less, about 1/3rd the CBD, than other study programs used.
Regardless, the conclusions were remarkable.
The study found that of the 53 patients with infantile spasms or LGS, 92% had seizure reduction and 13% had seizure freedom. The only adverse effect reported more often after initiation of CBD was increased appetite. Many patients had improved sleep (53%), alertness (71%), and mood (63%).
Although these survey results “are nothing to scoff at,” they’re not evidence of efficacy, stressed Dr Hussein.
Notice the extraordinary side effects: improved sleep, greater alertness and enhanced mood. Not too shabby for a boutique oil.
MORE EFFICACIOUS?
Is CBD oil better, or more efficacious, than prescription medications? At this point it is too early to tell. Efficacy is how well drug A does in comparison to an equipotent dose of (a different category) drug B. Drug A is said to be more efficacious than drug B if it can quell a greater percentage of seizure activity than drug B. To do that we need formal studies which are underway, not online surveys.
Based on anecdotal reports, high CBD preparations are effective anti-seizure medications. As effective as most pharmaceuticals, and in special cases such as status epilepticus in Dravet syndrome, MORE effective.
Here, the research drug was Epidolex which is a nearly pure CBD pharmaceutical preparation. Note the dose here is much higher: 25 mg/kg body weight. That’s 1,000 mg CBD in a 40 kg patient. Let’s examine this in greater detail shall we?
Yet another study, an open-label, investigator-initiated trial of Epidiolex (25 mg/kg per day) in children and young adults with treatment-resistant epilepsy, was carried out by Orrin Devinsky, MD, also at New York University, and his colleagues.
The researchers collected efficacy data on 58 patients followed for 3 months. Of these patients, almost 40% had a greater than 50% reduction in seizures. For patients with Dravet syndrome, this reduction was just over 50% while for all other patients, it was about 30%.
Seizure freedom at 3 months was also highest for patients with Dravet syndrome (22%) compared with other patients (10%).
“These rates were much higher than we would expect from a placebo response alone,” noted Dr Devinsky…
Researchers followed 40 of the patients to 4 months and found no “drop off” in effectiveness from 3 months, said Dr Devinsky. “There does not appear, from this preliminary snapshot we have in this open-label study, that there is tolerance or loss of effectiveness over time.”
Again, the drug was very well tolerated, said Dr Devinsky. The most common adverse effects, reported by more than 10% of patients, were somnolence (19%) and fatigue (11%).
The “critical take-home message” from this study, stressed Dr Devinsky, “is that these are early promising results, but we need controlled trials to know how to move forward.[ref](http://www.medscape.com/viewarticle/837487) 06/22/2015[/ref]
The effect of adding CBD to patients taking anti-epilepsy drugs was investigated in an observational study of patients enrolled in an expanded access, compassionate use of CBD program.
These patients were also taking Epidolex which is a purified 98% oil-based CBD extract. Here, the dose was 10-20 mg/kg of Epidolex per day.[ref](http://www.medscape.com/viewarticle/837487) 06/22/2015[/ref]
So your average 40 kg child might be receiving 400-800 mg of medication per day. Contrast this to parents giving their children only 160 mg per day of CBD for their seizures (part two), and achieving excellent results.
This efficacious “low dose” CBD may be important if we find that the higher doses interfere too greatly with the metabolism of other drugs the patient may be taking.
CBD INTERFERES WITH DRUG METABOLISM
An important finding was that many of the patients witnessed an increase in their serum levels of two key anti-seizure medications: Valproic acid and clobazam.
Patients were on a background regimen of at least one to four medications in addition to CBD,” noted researcher Daniel Friedman, MD, assistant professor, New York University School of Medicine.
They found that levels of CBD were also elevated in addition to valproic acid and clobazam. About ¼ of the study participants on clobazam and about 1/3 of those on valproic acid needed their dose reduced.
If you or one of your children are on CBD, and you are taking other pharmaceuticals, be sure to have your serum levels checked of those other medications if any can become toxic at higher levels. Check in one month after starting CBD. If your source is through an artisanal preparation be aware that it is not the same thing as Epidolex.
Ben Whalley, professor, neuropharmacology, School of Pharmacy, University of Reading, United Kingdom, pointed out that artisanal preparations contain about 500 different chemical compounds, and many have high amounts of tetrahydrocannabinol, the psychoactive element of the marijuana plant.
In contrast, he said, preparations such as Epidiolex that are approved for clinical trials are 98% CBD and are specifically formulated as a conventional medicine.[ref]IBID[/ref]
MORE POSITIVE RESULTS
At Children’s hospital in San Diego, California, Dr Jeffrey Gold reports a case of a boy with Doose syndrome. It’s another rare disease which can morph into status epilepticus. This syndrome can eventually lead to learning problems and profound developmental delays if seizures are not controlled.
After juggling their child’s medication doses and still not happy with the results, the parents informally began daily CBD treatment from an unknown boutique source. Again they found that the CBD may have increased the patient’s levels of valproic acid.
Now comes the interesting part:
After valproate levels were lowered, the parents reported that their son had become seizure-free over about 4 months. Another EEG verified that the boy “was completely normal — honestly to our surprise,” said Dr Gold.
Although resolution of seizures and normalization of EEG have been reported before in Doose syndrome, and this can happen spontaneously or as a result of medication change, “it was very interesting that it happened shortly after the CBD was used, and then the valproate acid was normalized,” noted Dr. Gold.
Parents of children with seizure disorders should stay in the loop with their physician and be sure to tell him or her that you started giving your child CBD.
It looks as if CBD can interfere with the liver’s metabolism of many drugs not just anti-seizure medicines. This can become very important depending on the pharmaceutical being taken.
In summary, we have excellent early reports of CBD being an effective anti-seizure medication at varying doses. Furthermore, it appears that CBD may interfere with the metabolism of many drugs including anti-seizure medicines which could lead to toxicity mandating the checking of serum levels.
CBD’s most promising role may be in the treatment of several orphan diseases for which conventional anti-seizure medication has little impact.
Dr Hussein’s closing remarks were in reference to the titanic levels of bureaucratic red tape, and the frustration researchers must endure while cannabis still holds its absurd schedule 1 classification.
“It’s a tragedy that we’re being held back by bureaucracy when these patients, parents, and practitioners are so desperate,” commented Dr Hussein.
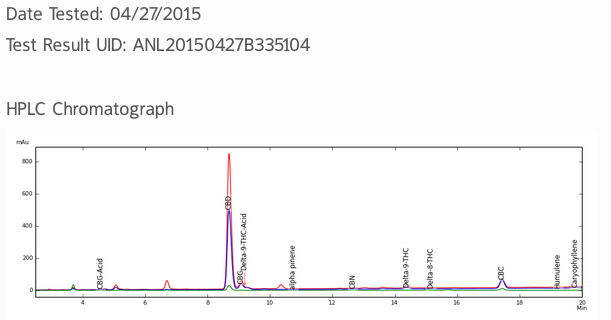
The Importance of Testing your CBD Products
The Importance of Testing your CBD Products
BUYER BEWARE: WHAT IS THE TRUE POTENCY?
In this article we’ll discover the stunning results of my requests for laboratory verification of commercial CBD products.
It is STANDARD for any legitimate company following good manufacturing practice (GMP), to provide verification of company claims. It should also be standard that consumers request it.
To my surprise not one company has provided me with that simple, basic requirement: proving your claim using a third party laboratory. Not one company!
If they cannot provide a sample copy for you, it’s because they know their merchandise is fraudulent. It’s that simple. A legitimate company should be proud or their product and be willing to prove their claims. For example, Zone Labs makes an excellent fish oil product which I have used for 17 years. The site provides a section where you can see every single batch’s third-party analysis of said product. They even refer you to the site (IFOS) where the testing is done!
In other words these well-known canna-businesses say they have high content CBD oil but we have to take their word for it.
One company had the hubris to send me a page that was simply created from scientific software that produces graphs! As a chemist, I could see that it was totally made up. They were trying to play me (and you) as befuddled children with no critical thinking skills.
Another company has a “real” looking printout on the front page of their glossy website claiming all batches are tested. I asked for said analysis, and all I got was a lab report that tested for contaminants which is also part of a total analysis package. Yet, no cannabinoid breakdown was provided. Of course, the lab did indeed test for cannabinoids but the company apparently didn’t want me to see it. I mentioned that to the company while putting in a second request.
Guess what? I never received a response. This “gotcha” moment revealed possible fraud and perhaps even criminal behaviour.
So far these businesses are failing the heat. They do not feel the need in providing proof. Instead we are to trust them and accept their claims on blind faith.
I don’t think so. Not when relying on them to cure you of a serious disease while stealing thousands of dollars from you!
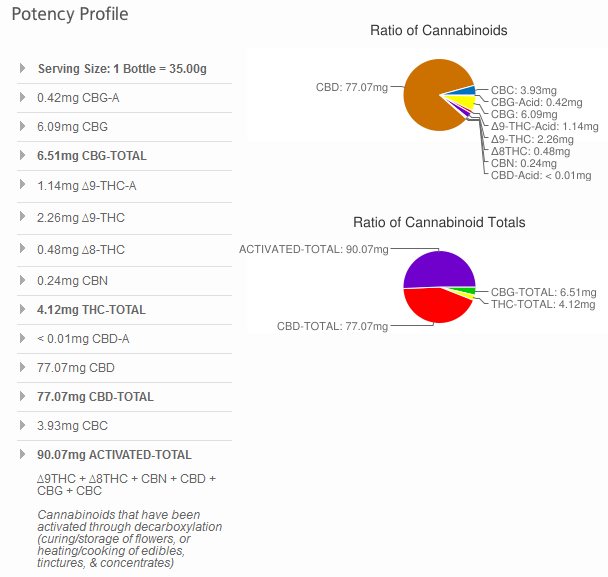
Real extracts (or any cannabis product) should be clearly marked with a percent concentration, or in milligrams per cc of vehicle for liquids.
For example, one decent company clearly printed on their label: contains 3.3 mg CBD per ½ dropper. One-half dropper is 0.4 cc according to their product label. Here you know exactly what you’re getting, at least from reading a clear label. They got that part right. Sadly, this same company does not provide third party proof.
Here’s a copy of the breakdown in potency of Sativa Valley’s CBD Tincture sample from Analytical 360’s analysis page followed by the cannabinoid breakdown.
There are other things tested for like terpenes, and contaminants that I have not provided.
Next observe the wonderful and novel labels (below) with their analysis printed right on the package of medical pot. This is refreshingly intelligent. This is also what SHOULD be included with all your purchases. This is a clear indication of third party testing and it should be standard.
Some of the most expensive CBD products on the market have only their website’s reassurance that they are what they say they are.
CBD oil could be anything. Raise the bar and demand proof or you may be wasting your money while encouraging a rapacious industry. This isn’t the old days when pot sellers were “a most happy fella.” Today we have businessmen, and with men of business comes a loss of ethics. Fraud easily follows.
In summary, demand:
1. An authenticated lab report with batch number, date, and % cannabinoids proving their claims.
2. A clearly written label with CBD dose in milligrams per serving.