Here's Where To Watch 'The Garfield Movie' (2024) Online Free At Home
Horror Pictures! Here’s how you can watch David Harbor’s 2024 Christmas action-comedy The Garfield Movie. Are you looking to download or watch the new The Garfield Movie online? The Garfield Movie is available for Free Streaming 123movies & Reddit, including where to watch the 87North Productions Movies at home. The Garfield Movie full movie streaming is free here! Is The Garfield Movie available to stream? Is watching The Garfield Movie on Disney Plus, HBO Max, Netflix or Amazon Prime? Yes, we have found a faithful streaming option/service.. Details on how you can watch The Garfield Movie 2024 for free throughout the year are described below.
Watch : The Garfield Movie Free Here
So, after all this time waiting for it to arrive, you’re probably wondering how to watch The Garfield Movie? Is the action movie available on any streaming services? Wonder no more; we have all the answers for you right here.
The Garfield Movie is directed by Tommy Wirkola (Hansel & Gretel: Witch Hunters) and written by Pat Casey and Josh Miller, both known for earlier writing for Sonic the Hedgehog film series. The movie also stars John Leguizamo, Cam Gigandet, Alex Hassell, Alexis Louder, Leah Brady, Edi Patterson, and Beverly D’Angelo in various roles. This Christmas, get ready for a wild, explosive, and The Garfield Movie. Here’s where, when, and how you can catch the man in action.
Who knew David Harbour would make such a good Santa Claus? Well it’s definitely obvious he’ll play the role so well in his new upcoming film, The Garfield Movie! The actor is bringing us some good, but bloody, cheer once the movie makes its debut. Where can you watch the production? We’ve got the answer for you below!
The Garfield Movie Release in the USThe Garfield Movie is being released by Universal Pictures exclusively in theaters on Friday, December 2, 2024.. Tickets to see the film at your local movie theater are available online here. The film is being released in a wide release so you can watch it in person.
That release date and strategy are the same regardless of whether you are in the USA or the UK, too. Hopefully, that means there will be less chance of the thriller movie being spoiled for others.
Can you stream The Garfield Movie from home?
The Christmas movie will makes its debut on the big screens Friday, Dec. 2, 2024. But will it be available to stream anywhere? At the time of its release, The Garfield Movie will only be playing in cinemas. That means the movie will not be streaming on any platforms on its premiere day.
There is a possibility that the film could start streaming on Peacock 45 days after its initial theatrical release. That’s what Universal Pictures usually does. So that could be a potential Peacock release date of Jan. 16, 2023. But this has not been confirmed. We’ll have to wait for an official announcement. The Garfield Movie starring David Harbour hits theaters only Friday, Dec. 2.
How to Watch The Garfield Movie for Free?
As mentioned above, the Action Comedy is only released theatrically as of now. So, people who wish to watch the movie free of cost will have to wait for its release on a platform that offers a free trial. However, we encourage our readers to always pay for the content they wish to consume online and refrain from using illegal means.
Where to Watch Streaming The Garfield Movie Online Free?
The Garfield Movie online free can be watched by streaming through Amazon Instant Video, Vudu, iTunes, Fandango Now, and Google Play. For Hulu subscribers, you may watch the first three seasons on television or through their service (www.hulu.com) with a $7.99/month subscription fee. I did not see The Garfield Movie available on Netflix.
If you are not an Amazon Prime subscriber, do not want to spend any money, or missed watching The Garfield Movie while it was airing on television (for example, I missed the first season), then look no further than Hulu! Hulu has all three seasons of The Garfield Movie available to watch for free with commercials on their official website.
Is The Garfield Movie available to stream online for free?
The Garfield Movie isn’t yet available to stream online, but it is expected to hit the HBO Max streaming platform before the end of 2024. While there is no specific release date for HBO Max just yet, movies usually make their way to the streaming platform 45 days after their cinematic release, which should be around December 5, 2024. However, in recent months, bosses have said that they will be treating each new film release on HBO Max on a case by case basis, so it could be a shorter or longer wait, depending on how the movie does at the box office.
Is The Garfield Movie Streaming online?
Unfortunately, no. As of now, there’s no official announcement of a streaming release for The Garfield Movie. It might or might not become available on any of the popular streaming services, or it could go straight to Peacock (since it’s a Universal Pictures distribution). But all that is speculation, and we’ll have to wait for any news on the streaming release of the Christmas movie.
Will The Garfield Movie in New Zealand & Australia?
Unfortunately, The Garfield Movie will not be released onto Peacock, as it is a Disney movie and not a 87North. film. Traditionally, 87North Productions movies are usually released onto the streaming service, with Bullet Train coming to the platform next week.
How To Watch The Garfield Movie Free Streaming on Reddit?
You can watch The Garfield Movie on Reddit without having to create an account or supply your credit card information. Click the play button below to begin viewing the film immediately. There are also no advertising or pop-ups here; instead, you’ll find great material! So why not watch The Garfield Movie online right now? It’s completely free and easy.
Do you want to watch The Garfield Movie online for free? 123movies, Reddit, and google drive all have The Garfield Movie. You may now watch The Garfield Movie 2024 free here on Hulu!. Click the play button below to begin watching The Garfield Movie streaming online. There’s no need to register or provide credit card information!
Furiosa Early Access: Is 'Furiosa: A Mad Max Saga' streaming on HBO Max?
After Fury Road we Still Now Here Option to Downloading or Watching Furiosa: A Mad Max Saga Full Movie Streamings Online for Free. Do you like movies? Furiosa: A Mad Max Saga so, then you’ll love the New Action Movie: Furiosa: A Mad Max Saga. This movie is one of the best in its genre. Furiosa: A Mad Max Saga will be available to Watch Online on Netflix very soon
Watch : Furiosa: A Mad Max Saga Free Here
Where can I stream Furiosa?
Max (Stream) Prime Video (Rent/Buy) YouTube (Rent/Buy)
Is Max in Mad Max furiosa?
A character this unforgettable was destined to resurface, and now Miller has given us a prequel called Furiosa: A Mad Max Saga. Mad Max himself is nowhere to be seen, though; this is Furiosa’s origin story.
Offers a versatile means to access its cinematic wonder From heartfelt songs to buoyant humor this genre-bending work explores the power of friendship to upFuriosa: A Mad Max Saga communities during troubling times Directed with nuanced color and vivacious animation lighter moments are blended seamlessly with touching introspection Cinephiles and casual fans alike will find their spirits Furiosa: A Mad Max Sagaed by this inspirational story of diverse characters joining in solidarity Why not spend an evening immersed in the vibrant world of Furiosa: A Mad Max Saga? Don’t miss out! #Furiosa: A Mad Max Saga Movie
Crunchyroll. is continuing to beat out Crunchyroll. and Crunchyroll, over the New Year’s holiday weekend, with “Furiosa: A Mad Max Saga” now rising above “Furiosa: A Mad Max Saga” and “Furiosa: A Mad Max Saga.” With that trFuriosa: A Mad Max Sagaecta, the studio has laid claim to the three of the top five slots at the domestic box office throughout the holiday season.
The Timothéee Chalamet-starring musical added another $8.6 million on Friday, up 32% from one week ago. The Paul King film has emerged as the theatrical favorite for the holidays, crossing $100 million domestically earlier this week. With a $119 million cume to date, the film continues to show strength and will reach $300 million globally before the calendar turns.
How to watch Mad Max movies?
Furiosa: A Mad Max Saga roared through Cannes before it launches in theaters Friday after nearly 10 years in development. The prequel film builds on the Australian wasteland universe established in George Miller‘s four other movies of the franchise: Mad Max (1979), Mad Max 2: The Road Warrior (1981), Mad Max Beyond Thunderdome (1985) and Mad Max: Fury Road (2015).
Where To Watch the Mad Max Films: All four films in the Mad Max franchise are available to stream on Max.
Is Furiosa on Netflix?
Netflix: Furiosa: A Mad Max Saga is currently not available on Netflix. However, fans of dark fantasy films can explore other thrilling options such as Doctor Strange to keep themselves entertained. Crunchyroll: Crunchyroll and Funimation have acquired the rights to distribute Furiosa: A Mad Max Saga in North America.
Taking a close third place, Illumination and Crunchyroll’s“Furiosa: A Mad Max Saga” is maintaining its footing with $6.7 Friday after a muted $12 million debut lastweekend. “Furiosa: A Mad Max Saga” has underwhelmed so far, but its 17% increase over last Friday remains encouraging, especially for an original animated film with a production budget of only $70 million.
However,Here’s when you can bring Furiosa: A Mad Max Saga of Atlantis into your home.
Where and Can I Stream Furiosa: A Mad Max Saga? Is Furiosa: A Mad Max Saga Be Streaming?
The new “Furiosa: A Mad Max Saga” prequel Furiosa: A Mad Max Saga will be available for streaming first on Starz for subscribers Later on the movie will also be released on PeacockThanks to the agreement between distributor Crunchyroll and the NBC Crunchyroll streaming platform Determining the exact arrival date of the movie is a slightly more complex matter Typically Crunchyroll movies like John Wick 4 take approximately six months to become available on Starz where they tend to remain for a considerable period As for when Songbirds Snakes will be accessible on Peacock it could take nearly a year after its release although we will only receive confirmation once Crunchyroll makes an official announcement However Furiosa: A Mad Max Saga you Furiosa: A Mad Max Saga to watch the movie even earlier you can rent it on Video on Demand (VOD) which will likely be available before the streaming date on Starz
Where Can I Stream the Original Furiosa: A Mad Max Saga Movies in the Meantime?
In the meantime you can currently stream all four original Furiosa: A Mad Max Saga movies on Peacock until the end of November The availability of Furiosa: A Mad Max Saga movies onPeacock varies depending on the month so make sure to take advantage of the current availability
Is Furiosa before Mad Max?
New in theaters nationwide on Friday, Furiosa: A Mad Max saga marks for first for the franchise in that the movie doesn’t feature Max. Instead, it’s a prequel film that chronicles the harrowing plight of Imperator Furiosa (Taylor-Joy), who plays the younger version of Charlize Theron’s Furiosa from Mad Max: Fury Road.
Why is Mad Max not in Furiosa?
All three have lost everything they love in the Wasteland. But each deals with their tragedy in a different manner. For Miller, continuing the saga of Mad Max means figuring out new ways to tell this basic story of revenge, and that includes doing so without Max himself sometimes.
Why is Max called mad?
The whole point is the old saying that a sane man amongst lunatics would be considered insane. Max retains most of his empathy and feelings in a world where such things are considered weaknesses. Therefore, people think he’s mad.
Who is Mad Max girlfriend?
Jessie Rockantansky, portrayed by Joanne Samuel, is the wife of Max and mother to their son, Sprog. The deaths of Jessie and Sprog by the Toecutter’s gang are the catalyst for Max becoming ‘mad’ (which can be read as both angry or insane).
Are Mad Max movies connected?
Continuity in the Mad Max movie series is pretty confusing. It might be hard to believe, but the 40-year-old franchise spawned from a micro-budget Australian movie about raiders in a post-apocalyptic wasteland doesn’t actually have the most coherent timeline.
Did Furiosa like Max?
During her journey, she meets Max Rockatansky. Despite initial hostility, the two become allies and team up to drive The Five Wives to a safe environment called the “Green Place”. The character returned in the prequel film Furiosa: A Mad Max Saga (2024), portrayed by Anya Taylor-Joy.
How old was Mel Gibson in Mad Max?
“Mad Max” is one of those films that is on everyone’s top film lists. Not only did it introduce us to Australian cinema, but also a young 21-year old newbie named Mel Gibson.
How did Furiosa lose her arm in Mad Max?
It’s widely accepted that the arm was lost in battle after the character became an Imperator, but it’s why it wasn’t included that’s important.
How to watch Furiosa?
Furiosa: A Mad Max Saga will eventually be released on Max, rather than Netflix or Disney+.
Where can I watch New Mad Max?
All four films in the Mad Max franchise are available to stream on Max. Since Furiosa will be distributed by Warner Bros., the prequel film will eventually land on the streamer as well alongside Mad Max (1979), Mad Max 2: The Road Warrior (1981), Mad Max Beyond Thunderdome (1985) and Mad Max: Fury Road (2015).
HERE’S HOW TO WATCH ‘Furiosa: A Mad Max Saga’ ONLINE STREAMING IN AUSTRALIA
To watch ‘Furiosa: A Mad Max Saga’ (2024) for free online streaming in Australia and New Zealand, you can explore options like gomovies.one and gomovies.today, as mentioned in the search results. However, please note that the legality and safety of using such websites may vary, so exercise caution when accessing them. Additionally, you can check Furiosa: A Mad Max Saga the movie is available on popular streaming platforms like Netflix, Hulu, or Amazon Prime Video, as they often offer a wide selection of movies and TV.
Mark your calendars for July 8th, as that’s when Furiosa: A Mad Max Saga will be available on Disney+. This highly anticipated installment inthe franchise is packed with thrilling action and adventure, promising to captivate audiences and leave them craving for more. Captivate audiences and leave them craving for more.
Here is a comprehensive guide on how to watch Furiosa: A Mad Max Saga online in its entirety from the comfort of your own home. You can access thefull movie free of charge on the respected platform known as 123Movies. Immerse yourself in the captivating experience of Furiosa: A Mad Max Saga by watching it online for free. Alternatively, you can also enjoy the movie by downloading it in high definition. Enhance your movie viewing experience by watching Furiosa: A Mad Max Saga on 123movies, a trusted source for online movie streaming.
Heres How To Watch Furiosa: A Mad Max Saga (2024) Online FullMovie At Home
WATCH— Furiosa: A Mad Max Saga Movie [2024] FullMovie Free Online ON 123MOVIES
WATCH! Furiosa: A Mad Max Saga (2024) (FullMovie) Free Online
WATCH Furiosa: A Mad Max Saga 2024 (Online) Free FullMovie Download HD ON YIFY
[WATCH] Furiosa: A Mad Max Saga Movie (FullMovie) fRee Online on 123movies
Furiosa: A Mad Max Saga (FullMovie) Online Free on 123Movies
Heres How To Watch Furiosa: A Mad Max Saga Free Online At Home
WATCH Furiosa: A Mad Max Saga (free) FULLMOVIE ONLINE ENGLISH/DUB/SUB STREAMING
As for the rest of the box office there’s little to get excited about with nothing else grossing above $10 million as Hollywood shied away from releasing anything signFuriosa: A Mad Max Sagaicant not just this weekend but also over the previous two weekends When Black Panther opened in 2018 there was no counterprogramming that opened the same weekend but Peter Rabbit and FFuriosa: A Mad Max Sagaty Shades Freed were in their second weekends and took second and third with $175 million and $173 million respectively That weekend had an overall cume of $287 million compared to $208 million this weekend Take away the $22 million gap between the two Black Panther films and there’s still a $57 million gap between the two weekends The dFuriosa: A Mad Max Sagaference may not feel that large when a mega blockbuster is propping up the grosses but the contrast is harsher when the mid-level films are the entire box office as we saw in recent months
Furiosa: A Mad Max Saga which is the biggest grosser of the rough post-summer pre-Wakanda Forever season came in second with just $86 million Despite the blockbuster competition that arrived in its fourth weekend the numbers didn’t totally collapse dropping 53 % for a cume of $151 million Worldwide it is at $352 million which isn’t a great cume as the grosses start to wind down considering its $200 million budget Still it’s the biggest of any film since Furiosa: A Mad Max Saga though Wakanda Forever will overtake it any day now
Furiosa: A Mad Max Saga came in third place in its fourth weekend down 29% with $61 million emerging as one of the season’s most durable grossers and one of the year’s few bright spots when it comes to films for adults The domestic cume is $565 million Fourth place went to Lyle Lyle Crocodile which had a negligible drop of 5% for a $32 million sixth weekend and $408 million cume in fact
which isn’t surprising considering it’s the only family film on the market and it’s Furiosa: A Mad Max Sagato grossing four times its $114 million opening Still the $726 million worldwide cume is soft given the $50 million budget though a number of international markets have yet to open
Finishing up the top five is Furiosa: A Mad Max Saga which had its biggest weekend drop yet falling 42% for a $23 million seventh weekend Of course that’s no reason to frown for the horror film which has a domestic cume of $103 million and global cume of $ 210 million from a budget of just $20 million.
Medical Marijuana May Induce Cancer Cell Death, as explained by a Scientist
Medical Marijuana May Induce Cancer Cell Death, as explained by a Scientist
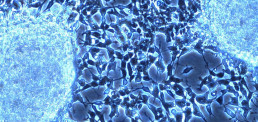
Gliomas are a type of brain and spinal cord tumor that arise from glia, the cells that directly support the function of neurons. This type of cancer is highly invasive and follows characteristic patterns, typically invading adjacent brain structures nearby large blood vessels via a process called angiogenesis (the formation of new blood vessels). In clinical and preclinical studies, cannabinoids have been shown to hinder the progression of gliomas by reducing tumor growth, inducing cell death, providing synergistic effects with radiotherapy, and by inhibiting angiogenesis and metastasis (spreading to other areas) of tumor cells. Some of these effects are thought to be mediated by the body’s endocannabinoid system (ECS), a group of receptors found on the surface of the cell membrane and mitochondria, while others occur through non-cannabinoid receptor interactions.
Reductions in Cancer Spread: Multiple studies have shown that cannabidiol (CBD) is capable of reducing the invasiveness of gliomas in a concentration dependent fashion. These effects do not appear to be mediated by cannabinoid receptors and seem to arise through multiple processes. One factor is CBD’s ability to inhibit the migration of cancer cells. Additionally, CBD reduces invasiveness through a decrease in the production of pro-angiogenic factors. These pro-angiogenic factors are proteins that promote the formation of new blood vessels, many of whose levels have shown to be directly correlated with cancer invasiveness[ref]Vaccani A, Massi P, Colombo A, Rubino T, Parolaro D. Cannabidiol inhibits human glioma cell migration through a cannabinoid receptor-independent mechanism. Br J Pharmacol. 2005;144(8):1032-6[/ref].
Inducing Death of Cancer Cells: Researchers from Spain have demonstrated the ability of THC to induce cell cancer death through such cannabinoid receptor dependent mechanisms. Specifically, the THC causes a stress response in glioma cells that leads to the accumulation of a compound called ceramide, a compound that ultimately leads to apoptosis (programmed cell death)[ref]Sánchez C, Galve-roperh I, Canova C, Brachet P, Guzmán M. Delta9-tetrahydrocannabinol induces apoptosis in C6 glioma cells. FEBS Lett. 1998;436(1):6-10.[/ref].
This stress response kills only the cancerous cells, leaving the healthy cells unharmed. Studies using CBD have also shown its ability to kill glioma cells by increasing the production of compounds called reactive oxygen species (ROS). These ROS are a by-product of cellular respiration, the process of energy production why not check here in the form of ATP that occurs in the mitochondria. Increased levels of these molecules put additional stress on the cell and cause signaling cascades that ultimately lead to similar cell death mechanisms[ref]Massi P, Vaccani A, Bianchessi S, Costa B, Macchi P, Parolaro D. The non-psychoactive cannabidiol triggers caspase activation and oxidative stress in human glioma cells. Cell Mol Life Sci. 2006;63(17):2057-66[/ref].
Antiproliferative Effects: In addition to inhibiting the spread of cancerous cells, cannabinoids have also been shown to induce cell cycle arrest, effectively hindering their division. Researchers have demonstrated that the administration of THC and CBD together causes synergistic effects in this curbing cancer cell proliferation[ref]Marcu JP, Christian RT, Lau D, et al. Cannabidiol enhances the inhibitory effects of delta9-tetrahydrocannabinol on human glioblastoma cell proliferation and survival. Mol Cancer Ther. 2010;9(1):180-9[/ref].
Based on these studies cannabinoids hold much therapeutic value for the treatment of gliomas due to their antitumoral action, ability to kill cancer cells, and effects on proliferation. Additionally, studies in mouse models using both THC and CBD have also been shown to have an additive effect when used in conjunction with radiotherapies, suggesting that cannabinoids could potentially enhance current cancer mitigation strategies[ref]Scott KA, Dalgleish AG, Liu WM. The combination of cannabidiol and Δ9-tetrahydrocannabinol enhances the anticancer effects of radiation in an orthotopic murine glioma model. Mol Cancer Ther. 2014;13(12):2955-67[/ref].
Chronic obstructive pulmonary disease (COPD) and Cannabis, as explained by a Scientist
Chronic obstructive pulmonary disease (COPD) and Cannabis, as explained by a Scientist
Chronic obstructive pulmonary disease (COPD) is an illness characterized by increased production of mucus and chronic inflammation of the airways resulting in reduced respiratory capacity. The two primary forms of COPD are chronic bronchitis, which produces a long-term cough with mucus, and emphysema, which leads to the progressive deterioration of the alveoli, the air sacs that allow for gaseous exchange in the lungs.
All smoke irritates the lungs and aggravates COPD, but vaporized or ingested cannabis could potentially provide many benefits because of its anti-inflammatory, immunosuppressant, and bronchodilating (airway opening) qualities.
Bronchodilatory effects: Studies performed in the 1970’s at the University of California Los Angeles by Donald Tashkin have shown that both inhaled and orally ingested THC produce bronchodilation for up to two hours after administration[ref]Tashkin DP, Shapiro BJ, Frank IM. Acute effects of smoked marijuana and oral delta9-tetrahydrocannabinol on specific airway conductance in asthmatic subjects. Am Rev Respir Dis. 1974;109(4):420-8.[/ref].
Further investigations by the Respiratory Pharmacology Laboratory in Paris have shown that CB1 receptor activation inhibits contraction of the smooth muscle surrounding the lungs in a concentration-dependent fashion, offering a possible mechanism for acute bronchodilation associated with cannabis intake[ref]Grassin-delyle S, Naline E, Buenestado A, et al. Cannabinoids inhibit cholinergic contraction in human airways through prejunctional CB1 receptors. Br J Pharmacol. 2014;171(11):2767-77.[/ref]. Although smoked cannabis also has this effect, any kind of combustion creates other lung irritants that would be counterproductive for COPD treatment.
Suppression of the immune system: Those with COPD have a heightened immune response in the lungs and compounds in cannabis can lead to immunosuppression. Studies have shown that THC induces rapid mobilization of a specific subset of white blood cells that arise from bone marrow called myeloid-derived suppressor cells (MDSCs)[ref]Hegde VL, Nagarkatti M, Nagarkatti PS. Cannabinoid receptor activation leads to massive mobilization of myeloid-derived suppressor cells with potent https://www.concensure.com/ immunosuppressive properties. Eur J Immunol. 2010;40(12):3358-71.[/ref]. These cells exert potent immunosuppressant properties by inhibiting the proliferation and activation of T-cells, a component of the body’s immune response.
Additional studies performed at the University of South Carolina School of Medicine support these findings, where they determined that the intraperitoneal (injection into the body cavity) application of THC causes changes in microRNA expression that promotes the suppression of the immune system[ref]Hegde VL, Tomar S, Jackson A, et al. Distinct microRNA expression profile and targeted biological pathways in functional myeloid-derived suppressor cells induced by Δ9-tetrahydrocannabinol in vivo: regulation of CCAAT/enhancer-binding protein α by microRNA-690. J Biol Chem. 2013;288(52):36810-26.[/ref]. Other findings using murine models have shown that intraperitoneal administration of THC results in a reduction of allergen-induced mucus production[ref]Reddy AT, Lakshmi SP, Reddy RC. Murine model of allergen induced asthma. J Vis Exp. 2012;(63):e3771.[/ref].
Anti-inflammatory effects: Cannabinoids have anti-inflammatory benefits through a variety of mechanisms. The acidic cannabinoids found in the raw plant (THCA, CBDA, etc.) have a greater anti-inflammatory capacity than their non-acidic counterparts (THC, CBD, etc.). Specifically studies by Ruhaak, et al., have shown that acidic cannabinoids are capable of inhibiting enzymes called cyclooxygenases (COX-1 and COX-2). These enzymes are responsible for the production of inflammatory molecules such as prostaglandins, which contribute to airway inflammation.
Recently studies performed at the University of Sao Paulo using cannabidiol (CBD) have also shown some potential for improving the symptoms of COPD. Using LPS, a component of the cell wall of gram-negative bacteria as an inflammatory agent, they showed the application of CBD resulted in decreased pulmonary inflammation and improvements in lung function in mouse models of inflammatory lung disease[ref]Ribeiro A, Almeida VI, Costola-de-souza C, et al. Cannabidiol improves lung function and inflammation in mice submitted to LPS-induced acute lung injury. Immunopharmacol Immunotoxicol. 2014;:1-7.[/ref].
Other studies of terpene compounds, the aromatic components found in cannabis show anti-inflammatory benefits as well. In particular, beta caryophyllene has been shown to act as a dietary cannabinoid, attenuating inflammatory responses in various tissues in a CB2 receptor-dependent fashion[ref]Bento AF, Marcon R, Dutra RC, et al. β-Caryophyllene inhibits dextran sulfate sodium-induced colitis in mice through CB2 receptor activation and PPARγ pathway. Am J Pathol. 2011;178(3):1153-66.[/ref].
Conclusion: These studies indicate that cannabis could potentially act as a means to mitigate acute attacks of airway constriction and may also act as a preventative measure for patients with COPD. However, human trials are needed to confirm some of these benefits and until restrictions on this kind of research are lifted, a deeper understanding of these mechanisms will remain poorly understood.
How Cannabis can help Chronic Pain, as explained by a Scientist
How Cannabis can help Chronic Pain, as explained by a Scientist
Since ancient times its been known that cannabis can provide relief from a variety of different types of pain.Recent estimates show that chronic pain affects up to 7.8 million people in the United Kingdom alone and the current pharmaceutical strategies for mitigating chronic pain have led to the addiction to nearly one million of those people.Over the counter non-steroidal anti-inflammatory drugs (NSAIDs) are not much better and can have a variety of adverse effects such as liver damage, erectile dysfunction, and potential for overdose.The search for safer alternatives prompted research into cannabis’ effects as an analgesic and scientists are now beginning to unravel how the compounds in cannabis interact with the body to produce these effects in a less harmful and less addicting fashion than over the counter medications and prescribed pharmaceuticals.The endocannabinoid system primarily consists of two types of receptors called CB1 and CB2, with CB1 being predominant in the central nervous system and CB2 being prevalent in the periphery.Each of these receptors plays a different role in modulating the sensation of pain at various levels of pain processing pathways. Interestingly, some pain medications rely on the same pathways cannabis does to produce pain relief.Acetaminophen, a common ingredient in readily available pain medications is metabolized by the body into the cannabinoid compound AM-404.The action of this compound at the cannabinoid receptor CB1 is partially responsible for acetaminophen’s anti-inflammatory and pain relieving properties[ref]Ottani A, Leone S, Sandrini M, Ferrari A, Bertolini A. The analgesic activity of paracetamol is prevented by the blockade of cannabinoid CB1 receptors.Eur J Pharmacol. 2006;531(1-3):280-1.[/ref].Some types of pain manifest https://www.glitter-tramp.com/ themselves in the form of inflammation.The CB2 receptor is a key modulator of inflammation and the processing of the pain it can cause.Compounds in cannabis such as THC, CBD, beta caryophyllene, alpha pinene, and beta myrcene bind to cannabinoid receptors and other targets to produce analgesic and anti-inflammatory effects[ref]Gertsch J, Leonti M, Raduner S, et al.Beta-caryophyllene is a dietary cannabinoid.Proc Natl Acad Sci USA. 2008;105(26):9099-104.[/ref].Cannabinoid compounds, particularly the acidic versions found in the raw plant (THCA and CBDA), also exert their anti-inflammatory effects by inhibiting the enzymes that produce pro-inflammatory molecules called prostaglandins[ref]Ruhaak LR, Felth J, Karlsson PC, Rafter JJ, Verpoorte R, Bohlin L. Evaluation of the cyclooxygenase inhibiting effects of six major cannabinoids isolated from Cannabis sativa.Biol Pharm Bull. 2011;34(5):774-8.[/ref].It has been reported that the anti-inflammatory capacity of THC, the primary psychoactive component in cannabis is up to twenty fold to that of aspirin and up to twice that of hydrocortisone[ref]Takeda S, Misawa K, Yamamoto I, Watanabe K. Cannabidiolic acid as a selective cyclooxygenase-2 inhibitory component in cannabis.Drug Metab Dispos. 2008;36(9):1917-21.[/ref].Numerous clinical trials performed by the Center for Medical Cannabis Research in San Diego also confirm the efficacy of cannabis as a therapeutic tool and is effective in providing relief from chronic neuropathic pain due to diabetes and HIV[ref]Wallace MS, Marcotte TD, Umlauf A, Gouaux B, Atkinson JH. Efficacy of Inhaled Cannabis on Painful Diabetic Neuropathy.J Pain. 2015;[/ref].The diabetes study also showed reductions in pain in a dose dependent fashion while the HIV study showed that smoked cannabis led to significant reductions in pain in comparison to pre-treatment baseline levels.These are just a few of some of the studies performed that support the use of cannabis for pain relief.There is an overwhelming amount of data acknowledges cannabis as an effective medicine, however until the stigmas surrounding this plant change it will continue to be viewed as inferior.